
The term pulp necrosis describes the death of the blood and nerve vessels within the tooth pulp, the pulp, which supplies the tooth with nutrients. The tooth is thus devital and is no longer supplied by the body systems, which is why it no longer feels any stimuli and neither reacts to cold, heat or pain. Pulp necrosis is irreversible and can only be treated with root canal treatment.The causes and forms are multiple. But does the diagnosis have an impact on a prognosis?
You might also be interested in: Building tooth
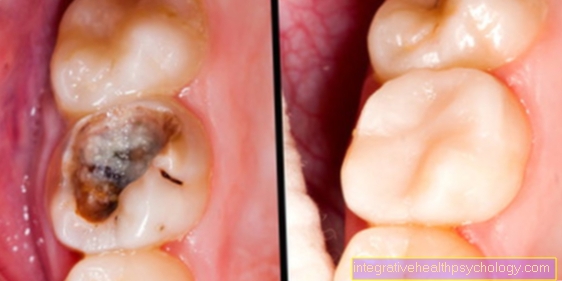
The causes of pulp necrosis are variable. If the tooth is infected by bacteria due to progressive caries, an infected pulp necrosis develops. The bacteria progress through the hard tooth substances until they have reached the pulp and attack the vessels and break away. The dead tissue is metabolized and inflammation can occur. This process was formerly known as corpse poison in the tooth.
$config[ads_text1] not found
This form of pulp necrosis can also be caused by a deepened gingival pocket. The deepened pocket indicates a widened periodontal gap. Since the gums are not so tightly attached to the tooth root, through this one can get to the root tip and the canal system.
The second irreversible form of the disease is sterile pulp necrosis. The cause is not the bacteria, but trauma and accidents. Furthermore, the forces during night grinding can be so strong that the pulp of individual teeth is irritated and the vessels within the tooth pulp die off.
You can also find important information at: Tooth pulp inflammation
In the event of accidents, the sterile form of pulp necrosis usually occurs. Hitting the tooth irritates it, so that the nerve vessels can die.
The most common example in the dental practice is therefore anterior tooth trauma. If the patient falls forward, the position of the upper jaw always causes the patient to fall directly onto the front teeth, which are the first to suffer pulp necrosis. It is noteworthy that a fall in childhood, which has remained without consequences for a long time, can lead to pulp necrosis symptoms decades later. However, it is not scientifically clear why this is the case. The knocking out of a complete tooth in toto can also lead to subsequent necrosis after a retransplantation, since the nerve vessels have been separated from the supply by the knocking out.
$config[ads_text2] not foundFor more information, see: Incisor broken off
A sterile pulp necrosis describes the loss of vitality of the tooth without bacterial influence. This can occur through trauma, for example through an accident combined with a fall or a blow to a tooth. Even decades later, childhood trauma can result in pulp necrosis. A sterile necrosis can remain asymptomatic and cause no discomfort for years. Often the sterile form is an incidental finding that arises from a cold test or an X-ray. The result of the diagnosis is a root canal treatment, which is initiated in the event of complaints.
An infected pulp necrosis is caused by bacterial influence and also robs the tooth of vitality. The big difference here is that the bacteria, which usually arise as a result of spreading caries, decompose and metabolize the vessels within the tooth pulp, which leads to discomfort. The unpleasant pain is caused by the fact that gases are created as degradation products in the metabolic processes of the bacteria, which cannot escape because the pulp is closed. There is an increase in pressure within the tooth, which the longer and more intensely the bacteria can metabolize, the stronger and more unpleasant it can become. The symptoms can only be alleviated by a root canal treatment, in which the canal system of the tooth is completely cleaned and disinfected so that all bacteria are removed. If the infected pulp necrosis is not treated, the bacteria will spread to over the tip of the root and can develop gangrene. The body's defense reaction, which does not manage to eliminate the bacteria in the canal system, causes an inflammation under the tip of the root, a so-called apical granuloma.
$config[ads_text2] not found
$config[ads_text3] not foundFor more information, see: Root inflammation
A tooth affected by pulp necrosis is diagnosed using clinical tests. This primarily includes the vitality test, during which a cold test is carried out. A healthy tooth feels the cold and reacts with a brief sensation, which disappears after a second or two. A tooth with pulp necrosis does not feel the cold because the nerve vessels in the pulp are dead and therefore feel nothing.
Furthermore, with advanced pulp necrosis, an apical granuloma may have developed that is also noticeable on a knock test. Percussion is painful on the tooth when the tooth is tapped with a blunt object. This pain can be explained by the fact that the tooth is pressed into inflammatory tissue. However, if the pulp necrosis has not progressed that far, the percussion test may be normal.
In the case of an apical granuloma, an x-ray may also show a lightening of the affected area, which was caused by bone breakdown by the inflammatory tissue. When the tooth is reamed, the dentist can also tell from a decaying smell and the color of the nerve tissue that the nerve has already been decomposed.
The symptoms that accompany an infected pulp necrosis are usually pain. The symptoms arise as pressure pain, as the bacteria that decompose the vessels produce gases that cannot escape. More and more gases are created the longer the bacteria metabolize the vessels and the pressure increases. The tooth can cause bite discomfort and pain if you touch it. Chewing on the affected side is also intolerable for the affected person. Furthermore, if the necrosis has persisted for a long time, the tissue below the tip of the root can swell and inflame, which leads to pain when touching. The affected area feels warmed up and looks red due to the increased blood flow. An unpleasant taste sensation is also possible if the putrefactive gases and secretions can get into the oral cavity through an enlarged gingival pocket. Pus and pus can also get directly into the oral cavity, which leads to bad breath, which can seriously affect the person concerned.
$config[ads_text4] not found
You might also be interested in: Inflammation of the gums with pus
Pain in pulp necrosis occurs primarily in the infected form due to the development of gas. This creates severe pressure pain, and throbbing is also possible. The patient experiences chewing and biting problems. Inflammatory pain around the affected root tip is also possible due to swelling and reddening.
In infected pulp necrosis caused by bacteria, the bacteria try to spread beyond the tip of the root and cause apical periodontitis there. The inflammation around the tip of the root occurs because the bone is broken down and the inflammatory cells infect and inflame the tissue. This can cause the tissue to swell and the signs of inflammation may cause pre-contact, which causes unpleasant symptoms.
The treatment of pulp necrosis consists of a root canal treatment. In the first step, a hole is drilled in the tooth that reaches up to the pulp. This creates direct access to the pulp through which primarily the pressure can escape. With particularly gangrenous teeth, the access also enables pus to drain away. The dentist tries to completely remove the inflamed and dead nerve tissue from the canal system with special files. The molars have a canal system made up of several canals from which any tissue has to be removed so that the symptoms disappear. In the next step, the sewer system is rinsed and disinfected to kill and remove the bacteria.
In gangrenous teeth, a medicated filler is placed in the system, which helps eliminate the bacteria and heal the tissue under the tip of the root. The next step is the preparation of the root canals. The canals are widened with ever larger needles and existing bends are straightened so that the canal system can be completely filled in the next step without any gaps. The last step is the root filling, which is only carried out when the tooth is completely symptom-free. The canal system is filled with thermoplastic root filling material, for example, in order to hermetically seal the disinfected system from the surrounding tissue. If the affected tooth remains symptom-free after the root filling, it can be prosthetically restored with a crown.
$config[ads_text1] not foundThe duration of pulp necrosis is variable. Progressive caries can very quickly reach infected pulp necrosis, trauma in childhood can only trigger sterile necrosis years later. The prognosis is good in both cases if a root canal treatment is carried out early on. Nevertheless, sterile necrosis is easier to treat due to the lack of bacteria, which is why the prognosis is better.