Melanoma in situ
General / Introduction
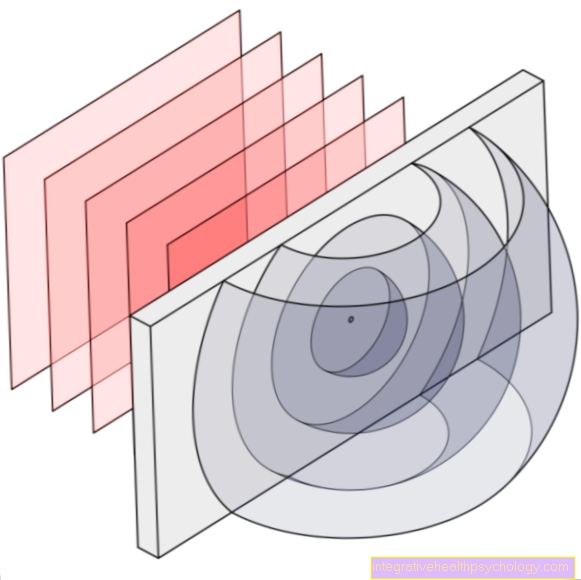
The melanoma in situ (syn. melanotic precancerous disease) is a preliminary stage of malignant melanoma. It is an increase in atypical melanocytes (Cells that are responsible for the dark hue) in the epidermis (epidermis). The atypical cells have not yet broken through the basement membrane, i.e. the membrane between the upper and lower skin. If left untreated, melanoma in situ can develop into malignant melanoma (malignant black skin cancer). There are several types of malignant melanoma. Melanoma in situ is not a specific type of tumor, but merely a description of the location and spread of the atypical cells.

Epidemiology
Typically this occurs Melanoma in situ only after the age of 50. As a rule, men are affected twice as often as women.
Other risks are:
- light skin type
- blonde or Red hair and
- longstanding strong Light exposure
Causes of Melanoma In Situ
The exact cause of melanoma development in situ is not known.
However, it is believed that the causes are similar to those of other skin tumors. Long-term UV exposure (sun exposure) is seen as the main cause.
For this reason, areas that are regularly exposed to UV radiation are particularly affected by melanoma in situ. These include the head, neck, forearms and lower legs. However, any part of the body can be affected. The DNA of the melanocytes is damaged by UV radiation.
If the body's repair mechanisms are no longer sufficient, a malignant new cell can arise. This grows outside of the normal regulatory mechanisms and thus continues to multiply unchecked.
Diagnosis
The diagnosis of melanoma in situ is usually dated Dermatologist posed. With the help of strong magnifying aids and a lot of experience, he can differentiate a melanoma in situ from a harmless mole.
To be on the safe side, a histological examination (tissue examination) of the Melanoma respectively.
This is the only way to determine the exact stage at which the tumor is to be determined.
Clinic (appearance of the melanoma in situ)
Over the years, the few cells turn into gray-brown to black-pigmented foci, which initially look like an ordinary mole.
These foci grow unrestrained, unevenly and without a sharp edge, which makes them different from harmless moles. Further symptoms usually do not occur, which makes melanoma difficult to detect in situ.
Therapy of melanoma in situ

Usually a suspicious mole is completely removed. The entire melanoma is always surgically removed in situ with a lateral safety margin and the small wound is then sewn again.
If there are many melanomas in situ, or if they are in unfavorable places, it is also possible to laser the melanoma in situ.
Another possibility is the removal by means of X-ray irradiation with a maximum radiation dose of 100 gray. However, if the melanoma is already advanced in situ and thus degenerated, radiation is no longer permitted.
forecast
If the melanoma is completely removed in situ on time, the chance of recovery is almost 100%.
If the melanoma has already developed further, lies in the Stage I. of malignant degeneration, the chance of recovery is still over 90%.
Summary
Melanoma in situ is a precursor to malignant melanoma.
It is probably caused by high and long-term UV exposure on areas of the skin that are particularly exposed to light. The melanoma in situ develops from previously healthy melanocytes and initially only grows as a gray-brown to black focus in the superficial layer of skin.
As a rule, adults over the age of 50, and especially men, are affected by melanoma in situ. If the melanoma is completely removed surgically or with a laser at an early stage, the chances of recovery are almost 100%.
If the melanoma is not removed early in situ, it can develop into a malignant skin tumor, the chances of recovery decreasing as the stage progresses.
In order to recognize such a melanoma in situ, a lot of experience and special examination equipment is necessary, so that cancer screening should take place regularly with a dermatologist.