osteoporosis
definition
Osteoporosis, which is also known as bone loss, is a disease affecting the skeletal system in which bone substances and structures are lost or greatly reduced. As a result of this reduction in bone mass, the tissue structure of the bone deteriorates and it loses stability and elasticity. As a result, the bones become more prone to fractures, in extreme cases a fracture can even occur without falling.
Due to the increased risk of breakage, the bone can collapse (sinter). This is particularly evident in the area of the vertebral bodies through visible changes. One example is the so-called “widow's hump”, which can be particularly evident in older women and can, under certain circumstances, lead to severe mobility restrictions.
frequency
During the menopause (= menopause) an average of about 30% of all women in Germany develop osteoporosis. It is therefore assumed that there are around four million patients across Germany.
Interestingly, there are big differences in the range of diseases in terms of origin. Studies have shown that blacks develop osteoporosis far less often than, for example, Europeans and / or Asians.
causes
There are a variety of causes for one osteoporosis, distinguishing between two forms:
- a primary (95%) and
- one secondary Form (5%) that arises on the basis of another underlying disease.
The human bone is made of that Bone tissuewhich by certain Minerals (mainly calcium and phosphate) that are stored in this tissue hardness and Strength wins.
It is important to know that the bone is one constant metabolism is inferior.
Until around the age of 30, the predominates construction of bones, then their breakdown. This process is mainly using various Hormones regulated.
Here play an important role:
- the Parathyroid hormone (a hormone from the Parathyroidwhich calcium detaches from the bone) and
- Calcitonin (a hormone from the thyroid) and Vitamin D (which ensure that calcium is built into the bones).
The effect of these hormones is modulated by the Sex hormones testosterone and estrogen. In the case of osteoporosis, this complex mechanism is disturbed at some point, so that the bone resorption becomes too strong, calcium is no longer stored in sufficient quantities, which means that the bones become attached density and thereby on strength loses. This makes it easier for bones to break.
Vitamin D deficiency
Diet can have a huge impact on the development of osteoporosis. Here, the vitamin D deficiency is a significant risk factor. In osteoporosis diagnostics, the activated vitamin D3 (= calcitirol) is determined by default with every blood sample. Vitamin D is a fat-soluble vitamin that is absorbed through food or is the only vitamin produced by the body itself. Reasons for a deficiency are, therefore, under / malnutrition, low UV radiation in winter, an absorption disorder despite sufficient intake with food and educational disorders due to poor liver or kidney functions. In addition to osteoporosis, a vitamin D deficiency in childhood leads to so-called “rickets” with disorders of growth and skeletal maturation. The function of vitamin D is, among other things, to promote mineralization and bone regeneration. In addition, vitamin D influences the metabolism of calcium, which in turn is considered a building block for bone formation: Vitamin D increases its absorption in the intestine and at the same time reduces excretion via the kidneys. In the prophylaxis of osteoporosis it is therefore very important to avoid a vitamin D deficiency.
Read more on this topic at:
- Vitamin D
- Vitamin D deficiency
to form
Osteoporosis can be divided into 2 main forms: the primary and the secondary form. The primary form occurs more frequently with approx. 90% than the secondary form with only 10%. The more common variant is divided into other types:
Type I osteoporosis is the term used to describe postmenopausal osteoporosis. Here, the low bone mass of the female sex is considered a predisposing factor. Senile osteoporosis is defined as type II and describes the fact that bone mass decreases with age due to less active or insufficiently working bone cells.
A third possibility is idiopathic osteoporosis, for which the exact cause is not known. It can occur either in children or adolescents or only in young adulthood. Male smokers in particular are at risk here. The secondary form includes various causes for osteoporosis. Systemic long-term therapy with certain drugs, especially glucocorticoids, but also proton pump inhibitors and anti-epileptic drugs plays a relevant role. Another important factor in the secondary form is immobilization: inactive people who do not move much or are bedridden for a longer period of time, the risk of developing secondary osteoporosis increases. Diseases that affect the hormonal balance and metabolism can also cause secondary osteoporosis. These include, for example, hypercortisolism or hypogonadism. What cannot be overlooked is the fact that an eating disorder due to a lowering of the estrogen level can also promote the development of secondary osteoporosis.
Read more on this topic at: Forms of osteoporosis
primary osteoporosis
The most common form of osteoporosis is the so-called postmenopausal Osteoporosis in women. It comes about because women in the Menopause Naturally, the level of estrogen in the blood is high sinks.
It is also common and one of the primary osteoporoses senile osteoporosisthat can be found in people (including men) over the age of 70, because this is where the Hormonal balance changes. Why, under the physiological circumstances, some people develop osteoporosis but not others, is still not fully explained.
In addition to the risk factors mentioned below, it is assumed that both genetic factors as well as behavior or external influences during adolescence have an impact on whether a osteoporosis forms or not (the late appearance of the first period or a permanent one Sedentary lifestyle are discussed here as risk factors, for example).
The third possibility of primary osteoporosis, and far less common than the two above, is this idiopathic osteoporosis. In these patients who are already in a younger age fall ill, it is still not known why this disease develops.
secondary osteoporosis
For thissecondary osteoporosis there are many different causes. On the one hand there are various hormonal disordersthat ultimately lead to osteoporosis.
These include:
- a Hyperthyroidism (Hyperthyroidism),
- an overfunction of the Parathyroid glands and a resulting excess of parathyroid hormone (Hyperparathyroidism),
- a Cushing-syndrome (Hypercortisolism) or one
- Malfunction of the Testicles (Hypogonadism).
Taking some medications can also trigger osteoporosis, for example long-term therapy with Cortisol (Mechanism as in Cushing's syndrome) or Heparin, Cytostatics, lithium, Vitamin K antagonists, Thyroid hormones or Aromatase inhibitors.
There are also diseases of Gastrointestinal tract: anorexia (Anorexia nervosa), Malnutrition and absorption (i.e. the Malnutrition), which ultimately all promote the development of osteoporosis by lowering the intake of important minerals below a necessary level.
In addition, some malignant diseases are also associated with osteoporosis, including myeloproliferative diseases (such as leukemia), Mastocytosis or that Multiple myeloma.
Other causes can be: underweight, a lack of folic acid or vitamin B12who have favourited Inflammatory Bowel Disease Crohn's disease and Ulcerative colitis, Diabetes mellitus, Kidney failure and some congenital diseases or syndromes such as the Ehlers-Danlos and the Marfan's Syndrome or the Vitreous bone disease (Osteogenesis imperfecta).
In addition, a bad lifestyle cause osteoporosis or at least favor its development. That means in detail that alcohol and Cigarette smoke, a poor diet (i.e. unbalanced, too few nutrients and Vitamins, too little calcium, too much phosphate, too little protein, too extreme diets) and not enough exercise are all important risk factors for osteoporosis.
Risk factors
In summary from the descriptions above, the following risk factors for the development of osteoporosis can be named:
- Family background
- Total operations in women
- Onset of menopause
- Calcium and / or vitamin D deficiency
- Too little movement
- Excessive cigarette, coffee and / or alcohol consumption
- Taking various medications (e.g. cortisone, heparin)
- Mental illnesses such as anorexia and bulimia
Symptoms
There are no typical osteoporosis complaints as such, since major complaints only arise, for example, as a result of the first bone fractures and thus in a more advanced stage.
With regard to an initial self-diagnosis, the fact that the first pain in the musculoskeletal system is of an uncharacteristic nature (e.g. "back pain") is made more difficult, the patient usually dismisses it as "harmless" and initially does not associate it with osteoporosis.
Read more on the topic: What kind of pain occurs with osteoporosis?
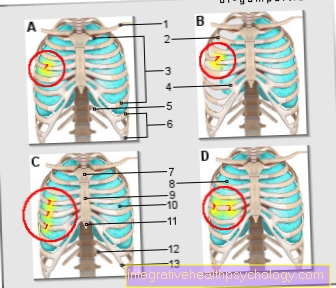
In principle, most osteoporosis-related complaints can be traced back to broken bones, which the patient may not even recognize as such. In the beginning, they are often rather undramatic and under certain circumstances can arise without recognizable external causes. In more advanced stages of osteoporosis, a strong cough can lead to broken ribs. In comparison, a healthy person would at least have to fall in order to cause broken ribs.
The following complaints can be seen as warning signs:
- Broken bones in the arms, legs and vertebrae (caused, for example, by stumbling over the edge of a carpet, by jerky movements or strong coughing) occur easily and possibly more frequently.
- An acute fracture can suddenly lead to severe pain (e.g. back pain).
- Muscle tension occurs as a result of the spine misalignment.
- External changes, such as the formation of a back hump, the loss of height by up to 30 cm become visible.
- Breathing difficulties due to restricted lung expansion or digestive problems due to constriction of the intestine, possibly also lumbago-like complaints due to pressure on nerves, sensory disturbances in the skin crystallize.
- Chronic and recurring back pain unexpectedly turns out to be older broken bones on x-rays
Information on bone density measurement can be found here.
Pain
The symptoms of osteoporosis are often unspecific. However, diffuse back pain is typical as an early symptom. In the further course, especially in the thoracic spine, the spine curves backwards (= kyphosis) with the formation of a hunched back. Due to these changes in the spine, the body size of osteoporosis patients decreases. The back pain then emanates from the bones on the one hand, but also from muscles and tendons in the further course, provoked by poor posture and relieving posture. The reason for the bone pain are so-called pathological fractures, i.e. broken bones without adequate trauma.
The location of the fractures varies depending on the type of osteoporosis: In the senile form, the femoral neck, upper arm or forearm are mostly affected, whereas in the postmenopausal form it is more the vertebral bodies. Accordingly, the pain occurs not only in the back but also at the above-mentioned predilection sites. Changes in the spine can also irritate the nerves emerging from the spinal canal. These can manifest themselves as nerve pain that can be triggered by pressure or as lumbago-like pain. Since the pain is ultimately based on fractures in most cases, additional symptoms will occur. This includes restricted mobility and functional losses. When the vertebral bodies are affected, there is also a loss of size.
However, pain can also occur as a side effect in the context of osteoporosis therapy. Taking the drugs "desonumab" and "parathyroid hormone" may cause pain in the limbs. In general, pain in patients with osteoporosis should always be perceived as a warning signal, as it usually indicates a pathological fracture. Since there is a risk of chronic pain in osteoporosis patients, value should be given to timely pain therapy.
Read more on this topic at: What kind of pain occurs with osteoporosis?
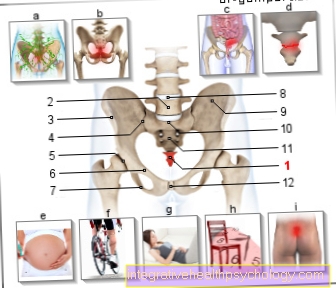
Osteoporotic femoral neck fracture
In most cases there are initially no physical signs of osteoporosis. As a rule, this disease only becomes noticeable when the initial stage of the disease has already gone through, i.e. bone loss has already started and the first bone fractures have already occurred as a result. Due to the relatively high load, the bones break particularly often in the area of, for example:
- Hip,
- Forearm,
- Thigh neck or in the area of the spine.
A very common side effect of femoral neck fractures, which are usually caused by falls from the side, are fractures in the wrist area, which are caused by instinctively trying to catch falls.
In the advanced stages of osteoporosis. A slight slip, a slight twist or even carrying a heavy shopping bag is all it takes to break the vertebrae (vertebral body fracture). Coughing can also cause broken ribs in these advanced stages.
Since bone formation and breakdown are not equally weighted in the case of osteoporosis, the healing of the fractures is also quite difficult. There are patients whose bones never recover from fractures, so that under certain circumstances they may need long-term care.
As mentioned above, osteoporosis manifests itself through changes in appearance. Examples include the so-called "hunchback", also called "humpback" or even "widow's hump", and the "shrinking" of older people, ie the decrease in body size by several centimeters. Women are more often affected by these problems than average.
Further information on this topic is also available at: Femoral neck fracture
and
You can also find more information on this topic at: femoral neck fracture
Diet for osteoporosis
In the osteoporosis plays both under the prophylaxis as well as within the treatment nutrition plays an extremely important role.
If you have risk factors for osteoporosis or if you already have a disease, you should abalanced diet worry, which means all the necessary Vitamins, Minerals and Trace elements be ingested sufficiently but not too much with food.
In addition, radical diets and both overweight and underweight should be avoided if possible.
Since this disease is on a increased fragility is based on bones, it is of great importance that the bones are strengthened (again) from the inside out as best they can. In addition to a regular physical activity and possibly the medicinal Therapy, nutrition is a crucial pillar with which one can favorably influence the development and course of osteoporosis.
One of the most important components of bone is calcium, which ensures that the bone is attached density and hardness wins. Hence is a calcium-rich diet indicated if you want to prevent osteoporosis or if you already suffer from this disease.
Ideal are about 1500 mg Calcium per day, if this amount is exceeded by far, can in turn have a negative effect on bone metabolism.
Very much calcium is contained in:
- Dairy products (Milk, practically all types of cheese, yoghurt and quark),
- green vegetables (especially in kale, broccoli, fennel and leek),
- some Herbs (Dill, parsley),
- in some Types of fish and more and more often also in
- Mineral water (up to 500 mg in just one liter).
One must also remember that the need for calcium in women is in the pregnancy and during the Lactation and is also increased in adolescents.
A sufficient intake of is also crucial in osteoporosis Vitamins.
This is especially important Vitamin D3, which is involved in bone formation and also the absorption of calcium from the gastrointestinal tract. In order to ensure a sufficiently high concentration of this vitamin in the body, on the one hand it is important to eat it (there is a lot of vitamin D in fish and Dairy products) and secondly, that you can spend at least half an hour a day in the Sun stops (this also includes staying under a cloudy sky), there UV radiation is necessary to convert this vitamin into its active form in the body.
But other vitamins are also essential necessary elements a diet for osteoporosis:
- namely vitamin C (in vegetables and fruits),
- Vitamin K (also in vegetables),
- Vitamin B6 (in whole grain products) and Trace elements (Fluorine, copper, zinc, contained in whole grain products, nuts and oat flakes)
Some acids like Apple- and citric acid (which can be found in various types of fruit) and Lactose (Lactose) are able to increase the absorption of calcium from the intestines.
That should be avoided
In osteoporosis, other substances should largely be removed from the diet to brush:
This is particularly important phosphate. This lowers the calcium level in the blood and thereby also the calcium that is available to be built into bone tissue.
Phosphate is found in large quantities in flesh- and Sausage products and also in Processed cheese. It is also contained as an additive in many foods and is then labeled as E 338.341 and E 450 on the packaging.
Some acids, especially Oxalic acid, which can be found in rhubarb, Swiss chard and spinach bind calcium (and also other minerals) in the intestine and prevent it from being absorbed here. Consequently, these products should not be over-consumed either.
Another important aspect of nutrition for patients with osteoporosis is Protein intake. On the one hand, it has been shown that the uptake of protein also helps build bone tissue support can.
On the other hand, too much intake (especially of animal protein such as meat, which contains a high number of sulfur-containing amino acids such as methionine and cysteine) is accompanied by a drop in the pH value in the urine. This change makes the Increased excretion of calcium.
Have a similar effect alcohol and caffeinethat is about inhibiting the secretion of the hormone Adiuretine (ADH) to an increased excretion of fluid and thus also of calcium cause.
Bad is also the supply of osteoporosis too much Table salt, which is a lot sodium contains. Sodium promotes the excretion of calcium by the kidneys and should therefore be absorbed never five to six grams exceed per day. Again, you should take a look at the label of a Mineral water bottle Throw in, as some water contains very high amounts of sodium (200 mg per liter should never be exceeded)! Otherwise, we recommend using when cooking and seasoning Iodized saltwhich is enriched with fluoride.
Among other things, for the reasons described above, one should be careful with osteoporosis not to consume luxury foods such as alcohol (In addition, for many, excessive alcohol consumption ultimately leads to a Insufficient supply, especially vitamins and trace elements), caffeine (Coffee, cola, black tea) and To smoke cigarettes keep it on a low level.
The nicotine contained in cigarette smoke makes it worse Blood circulation of bone tissue and also promotes the breakdown of female sex hormone estrogen. These two mechanisms ultimately promote the development of osteoporosis.
treatment
Osteoporosis is currently both underdiagnosed and under-treated in Germany. An optimal therapy is considered to reduce mortality.
The therapy is divided into osteoporosis and fracture prophylaxis and drug therapy. Basic therapy recommends physical activity to strengthen muscle strength as well as optimal nutrition to reduce the risk of osteoporosis and the associated fractures. Alcohol and nicotine abuse should be avoided. An adequate intake of vitamin D3 and calcium is also prescribed. If necessary, both substances must be supplemented with medication, as they play an important role in bone metabolism and thus have an influence on the development of osteoporosis.
Part of the prophylaxis is also to reduce the risk of falling. This can be achieved by stopping sedating medication or by using walking aids. Heat therapy and heliotherapy have also shown positive results in osteoporosis therapy. Psychosocial support is also recommended. The second important part of osteoporosis treatment is drug therapy. Bisphosphonates are the first choice drugs. Other drugs include raloxifene, strontium ranelate, denosumab and parathyroid hormone. Overall, the therapy lasts at least 3 to 5 years, with the exception of the drug parathyroid hormone, which may be administered for a maximum of 24 months. During the treatment, regular re-evaluation and follow-up to determine the further therapy is essential. This assessment should be based on the current guidelines.
Read more on this topic at:
- Bisphosphonates
- Therapy of osteoporosis
- Prevent osteoporosis
Medication
Drug therapy is considered a special therapy and is based on 2 principles: on the one hand, antiresorptive and, on the other hand, anabolic therapy. Antiresorptive means that drugs are used that inhibit the breakdown of bones by certain cells (so-called osteoclasts). These include drugs such as bisphosphonates, estrogens, SERMs such as raloxifene (= selective estrogen receptor modulator) and denosumab. With the help of anabolic therapy, bone building is to be promoted. Such stimulation is achieved by the parathyroid hormone.
All of the drugs mentioned are class A drugs because they significantly reduce the risk of fractures in the presence of osteoporosis. The indication for drug therapy should be made as soon as certain criteria are met. These include, among other things, low bone density, the presence of risk factors, old age. In addition to the standard drugs mentioned, there are others such as fluoride and calcitonin. Fluoride promotes bone formation, calcitonin inhibits bone loss.
Bisphosphonates
The bisphosphonates are the first choice drug for osteoporosis. They show an antiresorptive effect in that they inhibit the bone-degrading cells (= osteoclasts). This can lead to an increase in bone density. Regular intake of bisphosphonates can reduce the incidence of fractures by up to 75%. Alendronate, risedronate, ibandronate and zoledronate are available as preparations. The latter preparation only needs to be taken once a year. With the other preparations, you can choose between daily and weekly dose intake.
Bisphosphonates are contraindicated if there are diseases of the esophagus such as strictures or varices or if patients have gastric ulcers.Existing renal insufficiency (GFR <35ml / min), pregnancy and a calcium level that is too low also prohibit the use of bisphosphonates. Discomfort in the stomach and intestinal tract can be an undesirable side effect. Aseptic bone necrosis of the jaw is also possible. This side effect is more likely to occur when bisphosphonate is administered intravenously as part of tumor therapy. To prevent undesirable side effects such as inflammation of the esophagus, care should be taken to take the bisphosphonates in the morning and at least 30 minutes before eating. The purpose behind this is to avoid complex formation with calcium. In addition, it should be taken with sufficient fluids and in a sitting position.
diagnosisThe diagnosis of osteoporosis is made as a combination of anamnesis, clinical examination and technical measures. In the anamnesis it is important to inquire about the level of physical activity and to document the exact medication plan. Certain medications, as well as low physical activity, increase the risk of osteoporosis. Women should also be asked about the time of menopause, as the associated drop in estrogen levels can also provoke the occurrence of osteoporosis. In the context of osteoporosis there is a reduction in body size so that regular measurements can provide an initial indication of overt osteoporosis. In the physical examination, the so-called "fir tree phenomenon" can also be recognized in many patients: These are folds of skin on the patient's back that run downwards like a fir tree from the center of the spine, so they are reminiscent of a fir tree train due to decreasing body size.
Various parameters can be measured after a blood sample has been drawn. Particular attention should be paid to values such as alkaline phosphatase, calcium, phosphate, creatinine, vitamin D, etc. Some of the values are also used to rule out various differential diagnoses. In addition, hormones such as TSH as a thyroid hormone and certain values in the urine can be determined to detect the first signs of osteoporosis.
X-rays on the one hand and so-called osteodensometry on the other hand are available as apparatus for making the diagnosis. There are various criteria on the X-ray that indicate the presence of osteoporosis. This includes, for example, increased radiation transparency of the bones, which means that the bone is less dense. In addition, possible vertebral body fractures can be shown very well in the X-ray.
Read more on this topic at: Diagnosing osteoporosis
test
The diagnosis of osteoporosis can be verified using a test. This test includes a bone density measurement and is also known in technical terms as a so-called osteodensometry. The best known method is the measurement of the density of the bone area (unit in g / cm2) and is known as "Dual X-ray Absorptiometry (= DXA). Other possible methods include quantitative computer tomography (= QCT), in which, in contrast to DXA, the real physical density is measured (unit in g / cm3) and quantitative ultrasound (= QUS). Compared to the other tests, the last-mentioned method shows no radiation exposure. In a broader sense, the so-called “time up an go” test, the “chair rising” test and the tandem stand can also be used to determine the risk of falling in high-risk patients. These test results can be used to assess how mobile the patient is and how high the risk is of falling during everyday movement tasks, which in the case of existing osteoporosis is inevitably associated with an increased risk of fractures due to the lower bone density.
Read more on this topic at: Bone density measurement
DXA
DXA stands for "Dual X-ray Absorptiometry". With the help of X-rays, the surface density of the bone mineral content can be calculated (g / cm2). The measurement is carried out on the lumbar spine (lumbar spine 1-4), on the thigh bone near the trunk and on the thigh bone. The minimum values of all 3 measurements are decisive. The presence of osteoporosis is then defined using two scores. The so-called T-Score describes the standard deviation (SD) from the mean value of the maximum bone density compared to a 30-year-old, healthy person of the same sex. If the T-Score is more than 2.5 SD below the norm, one speaks of osteoporosis. The preliminary stage of osteoporosis, osteopenia, is defined as having a T-score of 1 to 2.5 SD below the norm. As soon as a fracture occurs in addition to the more than 2.5 SD below the norm, one speaks of overt osteoporosis. In addition, risk factors such as smoking or immobilization have an influence on the T-Score: If there is an additional risk factor, the T-Score is increased by 0.5, and with 2 or more risk factors even by 1.0.
Read more on this topic at: DXA measurement
Prevent osteoporosis
The prophylaxis of osteoporosis is just as essential as an optimal therapy. Various measures are available for prevention. Lifestyle and diet are an important aspect. Since, in contrast to many other diseases, a higher BMI is considered protective, care should be taken to ensure a sufficient intake of calories (BMI approximately> 20kg / m2). A daily intake of calcium (approx. 1000 mg), for example in the form of effervescent tablets, is also recommended. In addition, it is important to be in the fresh air for at least 30 minutes a day and ideally in the sun to ensure vitamin D3 formation. Otherwise, an additional intake of vitamin D3 supplements is advisable. Vitamin B 12 and folic acid should also be sufficiently absorbed with food. Smoking is considered a risk factor for osteoporosis, so nicotine abuse should be avoided. There is also the need to monitor the medication plan and, if necessary, adjust it or switch to other preparations.
A handful of drugs increase the risk of osteoporosis, especially with long-term therapy. These include above all glucocorticoids, but also anti-epileptic drugs, antidepressants, sedating drugs or proton pump inhibitors. Since osteoporosis mostly affects the elderly, osteoporosis prophylaxis also includes preventive measures such as regular physical activity and avoiding prolonged periods of immobilization. The aim is to improve both muscle strength and coordination. In addition, good physical activity and basic fitness alone reduce the risk of developing osteoporosis, as a lot of exercise promotes the development of bone mass. For patients older than 70 years, a precise history of the fall should also be carried out: This means that the exact causes of past falls should be inquired about and any avoidable reasons should be treated accordingly. Since the hips are particularly at risk in a fall, wearing hip protectors is a preventive measure. The use of walking aids or a rollator are also helpful. Further supportive measures are warmth and heliotherapy.
Read more on this topic at: Prevent osteoporosis
Can Osteoporosis Be Cured?
When answering the question of whether osteoporosis is curable, opinions differ. If one looks at the overall picture of the disease, osteoporosis is not considered to be completely curable, since the previous bone condition can never be achieved despite optimal therapy and any fracture events that have taken place cannot be reversed. Healing would mean that the entire bone mineral balance could be restored and that pathological fractures associated with osteoporosis would have to be healed optimally and without permanent restrictions. The last aspect mentioned is difficult to achieve, especially in old age. Nevertheless, there are also advocates of the opinion that osteoporosis is curable. However, the restriction must be made here that it is an early stage of osteoporosis without the presence of pathological fractures. Then a temporary disturbance of the bone mineralization can be brought back to normal through optimal therapy with sufficient vitamin D and calcium intake, sufficient exercise and appropriate medication. It is therefore not possible to make a generalized statement as to whether osteoporosis is curable or not. It is always important to assess the individual clinical picture depending on the stage and the existing risk factors and to use this information to decide whether the osteoporosis is curable or not.
Summary
In a healthy person, bone formation and breakdown are in a harmonious balance. This means that as much bone builds up as was previously broken down in any way. In osteoporosis patients this balance is disturbed.
If too little bone is built up, or if the degree of bone loss deviates from the norm, there is a loss of substance, which makes the bone less resilient and thus more prone to breakage.
Due to this disharmony in the balance between bone formation and breakdown, in combination with the restructuring of the bone substance, the patient's ability to move can be impaired.
In addition to the general loss of quality of life, caused by the restricted mobility, the increased risk of bone fractures plays a particularly important role. Other symptoms may also arise, such as:
- Circulatory problems,
- a general deterioration in general well-being,
- as well as cease psychological stress.