Urinary tract
Synonyms in a broader sense
- Renal pelvis
- Ureter
- ureter
- urethra
- Urinary tract
- Primal entrance
- kidney
- bladder
Medical: ureter, vesica urinaria
English: bladder, ureter
introduction
The draining urinary tract includes the renal pelvis (pelvis renalis) and ureters (ureter), which are lined by specialized tissue, the so-called urothelium.
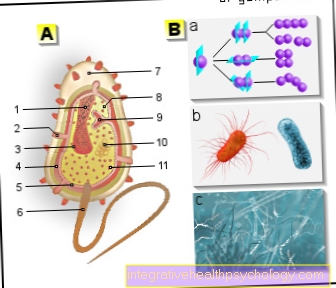
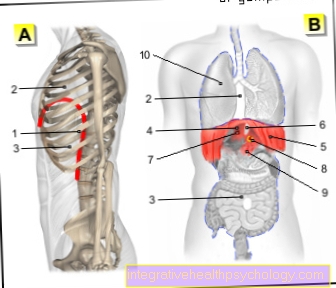
Urinary tract illustration
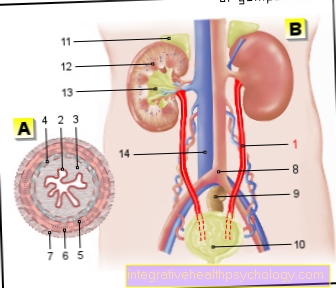
- Ureter - Ureter
- Transitional epithelium - Urothelium
- Shift layer of the
Mucous membrane - Lamina propria - Inner longitudinal layer -
Stratum longitudinal internum - Outer longitudinal layer -
Stratum longitudinal externum - Middle ring layer -
Circular stratum - Connective tissue covering with
Blood vessels - Tunica adventitia - Aortic fork - Aortic bifurcation
- Rectum - Rectum
- Urinary bladder - Vesica urinaria
- Adrenal gland -
Suprarenal gland - Right kidney - Ren dexter
- Renal pelvis - Pelvis renalis
- Lower vena cava - Inferior vena cava
You can find an overview of all Dr-Gumpert images at: medical illustrations
anatomy
1. Renal pelvis
It arises from the confluence of 8-12 kidney calyxes (calices renales), which enclose the kidney papillae and catch the urine. Depending on the arrangement of the calyxes, a distinction can be made between an ampullary (with short tubes and a wide renal pelvis) and a dendritic (with long, branched tubes and small renal pelvis) calyx system.
The calyx and pelvis are surrounded by a richly perfused connective tissue, which is also a network of smooth, i.e. H. contains unwillingly controllable muscle cells that regulate the size of the cavity system.
2. ureter
The 25 - 30 cm long ureter represents the connection between the renal pelvis and the urinary bladder. A distinction is made between:
- Pars abdominalis (abdominal section)
- Pars pelvica (pelvic section)
Both ureters cross the urinary bladder wall at an incline, which, together with the internal pressure of the urinary bladder, ensures that the mouth is usually closed in order to prevent the urine from building up. They are opened when a wave of contraction of the ureter arrives. Muscles arranged in three layers ensure that the urine is transported further into the bladder by means of peristaltic waves.
There are three bottlenecks in the ureter:
- at the exit from the renal pelvis
- at the crossover through the inguinal vessels (aa. iliacae)
- when passing through the bladder wall
From time to time a double ureter can appear, which unites at different heights to form a ureter. Separate openings into the urinary bladder can also occur. However, such anomalies are usually of no disease value and can go undetected for a lifetime.
The ureter (ureter), renal pelvis and calyx system can be visualized in the X-ray image (radiological) with the help of special contrast media, which are either administered via the vein and then excreted through the kidneys (intravenous pyelogram) or the contrast media is fed backwards via the bladder directly into the Ureter given (retrograde pyelogram).
The blood supply is ensured via branches of the renal artery (renal artery) and various other vessels, which form a dense network in the ureter wall.
The wall of the ureter consists of:
- Mucus layer (Tunica mucosa)
- Muscle layer (Tunica muscularis)
- outer top layer (Tunica adventitia)
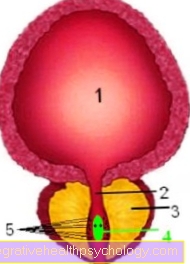
Illustration urinary bladder
Cross section through the bladder and underlying prostate:
- bladder
- urethra
- prostate
- Seed mound with the two openings of the spray tubules
- Excretory ducts of the prostate
In the bladder (Vesica urinaria) is a muscular hollow organ, the shape of which varies depending on the level of development or filling.
When slightly filled, the bladder is pyramidal with the tip tilted forward.
A distinction can be made between:
- Bladder tip (Apex vesicae)
- Bladder (Corpus Vesicae)
- Bladder base (Fundus vesicae) with the confluence of the ureters and the departure of the urethra
- Bladder neck (Cervix vesicae) going into the urethra (urethra) transforms.
The so-called trigonum vesicae (bladder triangle) is a triangular area free of mucous membrane folds between the junctions of the ureters and the beginning of the urethra. Here the mucous membrane is immovably connected to the underlying muscles. In men, the part of the bladder is directly below it prostate.
The wall construction and the attachment of the urinary bladder allow large fluctuations in volume.
The wall consists of:
- Tunica serosa: It consists of the peritoneum in the upper and rear areas of the bladder.
- Tunica muscularis: It contains three layers of smooth muscles (outside and inside lengthways, in the middle running across). The fiber strands merge into one another and form a functional unit (M. detrusor vesicae). The muscles in the area of the trigonum vesicae should be emphasized. It is only single-layered and wraps around the inner opening of the urethra like a kind of ruff. Thus it preserves the continence and in men the penetration of the ejaculate into the urinary bladder.
- Tunica mucosa: It consists of transitional epithelium. The height of the lining mucous membrane depends on the filling state, i.e. H. the thickness of the wall is approx. 1.5 - 2 mm when filled and approx. 5 - 7 mm after emptying.

Urinary bladder lining under the microscope
Without filling, the mucous membrane lies in folds, with increasing bladder filling the surface becomes smooth.
The urinary bladder is fixed by connective tissue in the area of the cervix and fundus. Otherwise it can be moved in order to adapt to different filling states. This is done by a different ligament apparatus in men and women. When expanding, the urinary bladder emerges from the anterior abdominal wall from the pelvis and at the same time pushes the corresponding peritoneum in front of it. If the filling is stronger, the symphysis line is exceeded, but the bladder usually never rises above the umbilical level.
The urinary bladder generally holds a maximum of 1500 ml, but the urge to urinate occurs at around 200-300 ml.
The internal opening of the urethra is normally closed by the muscles of the urinary bladder and by the continuous contraction (tone) of the internal urethral sphincter. This is controlled by a special nerve network.
When the bladder is emptied (micturition), a nervous signal is emitted from the fibers of the Parasympathetic nervous systemwhich pressurizes the contents of the bladder by tensing the detrusor vesicae muscle. The bladder neck opens by pulling its anterior wall forward through the pubovesicalis muscle, which is also activated. These processes cannot be controlled deliberately.
However, there is also a deliberately controllable occlusion, the M. sphincter urethrae (rhabdosphincter). This makes it possible to arbitrarily initiate the urge to urinate but also to interrupt it. The micturition itself takes place completely automatically, by a spinal cord reflex, which in turn by centers in the brain (so-called micturition center in the formatio reticularis) can be inhibited or promoted.
When emptied, the bladder lies broadly and in the shape of a bowl pelvic floor. During micturition, it assumes a spherical shape, with the detrusor vesicae closing concentrically around its contents.
In the newborn, the urinary bladder protrudes from the pelvis due to the greater spatial confinement. Later, when the space in the small pelvis increases, the bladder slips into the pelvic ring (Descensus vesicae).
The blood supply takes place through branches of the internal inguinal artery (A. iliaca interna) with
- Superior vesical artery (superior bladder artery) for the lateral bladder wall and bladder surface
- Inferior vesical artery (lower bladder artery) for the base of the bladder
The blood from the venous networks in the mucous membrane and muscles is collected in the plexus venosus vesicalis (venous plexus of the bladder), which surrounds the base of the bladder. From there, the blood is diverted either directly or via intermediate stations to the internal inguinal vein (internal iliac vein).
The nerve supply can be divided into different nerve plexuses with different tasks.
- Intrinsic nerve plexus: It is located in the bladder wall and adapts the tone of the M. detrusor to the filling status of the urinary bladder.
- Extrinsic nerve plexus: it contains the following fibers
- sympathetic fibers (motor supply of the M. detrusor)
- sympathetic fibers (tone of the vessels, muscles of the bladder neck)
- Somatic fibers: They are the part that can be controlled voluntarily and supply the external vesic sphincter muscle.



.jpg)