Skin graft
definition
Skin transplantation is the complete, surgical removal or detachment of healthy skin areas anywhere on the body (mostly inside of the thigh / upper arm, buttocks, back) with subsequent reinsertion of this removed skin at another location. It is now one of the most frequently used basic techniques in the field of plastic surgery.
The goal of the skin graft is that Covering larger, defective areas of skinthat are no longer due to conservative therapy or a simple one surgical suture can be locked. Skin grafts are also used for the therapy of wounds, the natural healing process of which would be very tedious and risky.
This can for example after acid burns, Burn accidents and chronic, therapy-resistant wounds be the case.
Important prerequisites for the success of the transplant are one infection-free, well-perfused recipient wound and a complete healthy donor tissue. According to observations, the closer the extraction site is to the wound that is to be covered, the better the aesthetic results are often.

Reasons for a skin graft
Major injuries after accidents and arterial or venous vascular diseases (open skin defects often on the legs, e.g. leg ulcers, are among the most common reasons that lead to open wounds, which can no longer be healed or closed by conservative or standard surgical therapy , "open legs"). Larger burn or caustic areas and large skin defects due to ulcers (e.g. decubitus = "Ulcer from lying down“, Diabetic ulcers, etc.) can require a skin graft.
It is therefore desirable to cover such wounds as quickly as possible, since large, open wound surfaces form entry portals for bacteria and are therefore easily prone to infections. In addition, the body continuously secretes protein-rich fluid into / via the non-healing wounds, which, depending on the size of the defect, can lead to increased or even life-threatening fluid loss. The natural function of the skin as a protective barrier is also lost in these areas, so that the tissue directly underneath is at risk and can be more easily damaged.
Types of transplants

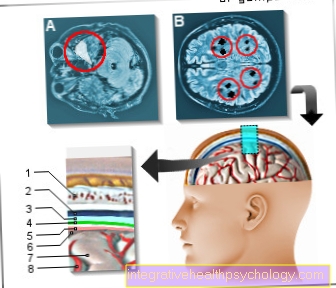
One distinguishes two different types of common transplants commonly used in plastic surgery: the Full skin graft and the Split skin graft.
Either so-called "Own transplants' (Autologous grafts / skin areas: the donor and the recipient are the same person) or but "Foreign skin grafts' (allogeneic grafts: the donor and recipient are not the same person) be used.
The latter method must always be used if more than 70% of the affected person's skin is damaged and one's own skin is insufficient to cover this large wound area.
In full skin transplantation, areas of skin are removed from the top two layers of skin (Upper skin / epidermis and the entire leather skin / dermis) and the Skin appendages (Hair follicles, Sweat glands etc.) exist.
These grafts are very thick compared to split-thickness skin grafts (0.8-1.1mm), the wound caused by the removal must be closed with a primary suture, which is why only smaller grafts can be taken.
In the process there is one Scarring in the extraction areawhich means that it can no longer be used for further removal. Despite slower growth, the cosmetic and functional result is significantly better than that of the split-skin transpants. This type of transplant is used preferred for deeper, smaller, non-infectious wounds.
The technique of producing a is also possible in the context of full-thickness skin transplantation Moving or swiveling skin flapWhenever there is intact, healthy skin in the immediate vicinity of the wound to be treated. In this technique, a flap of skin is attached three sides cut out and panned over the wound area and later attached. The advantage here is that the swivel graft maintains contact with the original skin area at one point, thus facilitating blood flow and growth.
Split skin grafts usually only contain the epidermis and parts of the dermis and are thinner (0.25-0.75mm) than full skin grafts.
The advantage that results from this is that the wound areas created by the removal are usually Heal spontaneously within 2-3 weeks and the donor area can even be used several times (In contrast to full skin removal, there is no scarring here).
For the removal of split skin, special knives (Dermatome, Humby knife), but it can also be done using another, special device, so-called "Mesh grafts' (Mesh grafts) by cutting the removed skin like a mesh. These then have 1.5-8 times the surface area of the skin area originally removed and thus enable particularly large wound areas to be covered. Other advantages of split-thickness skin grafts are that wounds with poor blood supply and not infection-free can be covered.
Another method for obtaining skin transplants is the cultivation of your own skin starting from individual, removed skin cells, which grow on artificial nutrient media within 2-3 weeks in the laboratory to form transplantable preparations.
Transplant technique
With split skin grafts, the donor skin area is under sterile operating conditions by means of Dermatome or Humby knife removed and, if necessary, reworked by the mesh-like incision and enlarged in its surface. The extraction point is cleaned and with hemostatic, the wound contracting Substances treated and sterile bandaged. The graft is applied to the recipient wound and fixed with tissue glue, staples or small sutures.
Full-thickness skin grafts are also removed under the same sterile operating conditions, but the classic scalpel is used for this and the removal site is previously marked using a template. Once the full skin has been removed, it will be completely degreased and, if necessary, several times with the scalpel scratched on the surfaceto get better growth later. The removal site is sewn up and covered with a sterile Compression bandage covered for about 5 days.
The application of the graft is similar to that of a split-thickness skin graft.
When removing full-thickness skin as well as split-thickness skin grafts, the plastic surgeon ensures that the Direction of the incision the course of the skin tension lines in order to ensure correct scar formation. Furthermore, it is taken into account that the transplant is incised in different places and not fixed too much and placed under tension, so that in the course of the Drainage of wound secretions is possible.
Depending on the size of the removal site and the wound to be covered, the surgical interventions are carried out under local or general anesthesia.
Healing and follow-up treatment of a skin graft
In order to ensure optimal healing of the transplant, the affected part of the body / extremity should be immobilized for 6-8 days in the first few days and regularly applied with slightly compressing bandages. As a rule, plaster casts or splints are used here.
Within approx. 10 days, the graft should be firmly attached to the newly formed tissue and connected to the blood supply system of the surrounding, healthy skin, so that sufficient blood flow to the graft is guaranteed.
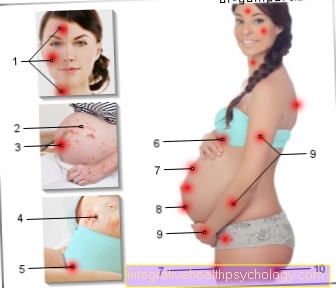
This is mainly made possible by the release of the skin's own growth factors. In some cases there may be swelling in the affected area within the first 2-4 days (edema formation through water retention or storage of wound secretion). With the blood flow, the color of the transplant also changes, which initially appears pale, after 3-4 days reddish, after approx. 1 week then red and finally after approx. 2 weeks it returns to the normal skin color. This is roughly the point in time when the hair starts growing again in the transplant area (approx. After 2-3 weeks).
In order to optimize the scar formation and to keep the less elastic scar tissue supple, care with fatty ointments can also help. The scarring that restricts movement should also be counteracted with exercise training to stretch the scar tissue, which should be started as soon as possible after the transplant has safely grown.
Skin graft complications
In contrast to foreign skin transplants, transplants using the body's own skin generally do not have any risk of rejection reactions. Complications that affect both self and foreign skin transplants are possible infections (mostly by "Streptococcus pyogenes") or bleeding during or after the procedure. Furthermore, healing disorders, delayed growth or even death of the transplant can occur if the covered wound does not have proper blood supply or sub-blood after the operation (Bruising) becomes.
Incorrect hanging up (undervoltage) or the lack of fixation (too loose) of the graft, can lead to difficulties in healing, as in this case there is no optimal contact between the graft and the wound bed.
Once the wound has healed, in some cases there may be changes in sensation or even numbness over the transplant area, as well as changed or missing hair growth in this area. In the case of very large transplant areas, the inevitable scarring process can lead to restricted movement of the affected limbs (above all about joints) because scar tissue is less elastic and stretchable.
The level of risk for possible complications depends on the one hand on age and on the other hand on accompanying secondary diseases that lead to poor wound healing. In particular, elderly patients (> 60 years) as well as newborns and small children at a higher risk of suffering complications, as well as patients with diseases such as diabetes mellitus, anemia, arterial circulatory disorders, immune and immune system disorders or chronic infections.
The use of certain medications can also influence and disrupt wound healing (e.g. anticoagulants, substances that suppress the immune system, anti-cancer drugs), as can poor nutritional status and regular nicotine consumption.