Epidural anesthesia
Definition of epidural anesthesia
Epidural anesthesia (PDA) is one of the regional anesthesia and is used to relieve pain in certain areas of the body. This is mainly used when surgery is to be performed in this region of the body. In addition, epidural anesthesia can be used to ensure freedom from pain during the first few days after an operation.
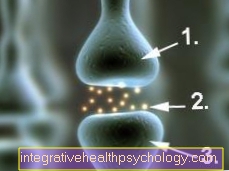
The term epidural anesthesia is derived from the Greek. The words "Peri" = "next to, around" and "dura" = "hard" refer to the anatomical area on which the drug is supposed to work: This is done using a needle or a thin tube in the room around the hard Spinal cord skin injected around.
This space is called the epidural space and is in close proximity to the spine.
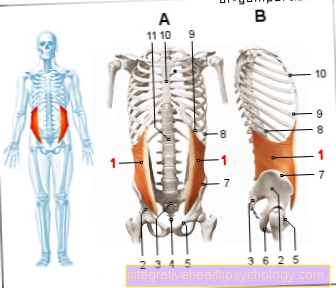
The area in which the sensation of pain is switched off depends on the anatomical puncture point on the back: To eliminate the sensation of pain in the area of the upper abdomen, an injection at the level of the (upper) thoracic spine and for anesthesia of the legs an injection in the area of the ( lower) lumbar spine necessary.
How painful is epidural anesthesia?
In the case of epidural or epidural anesthesia, an injection is made with a fine needle for local anesthesia. This is usually the most painful part of the procedure. The local anesthetic is distributed in the area to be punctured and also in the deeper layers.
After a short exposure time and consultation with the patient, the actual puncture takes place to numb the area to be operated. With this puncture, the patient should then "only" feel a feeling of pressure and no more pain.
In the case of difficult anatomical bone conditions in the area of the spine, several attempts may be necessary to reach the desired area. However, this is only done under adequate local anesthesia. If the injection needle touches the bony vertebral bodies during the puncture, a brief pain may result. The goal is to deliver the anesthetic directly to the area around the spinal nerve roots. Since these can also be touched briefly by the needle, there may be an “electrical sensation” or a “tingling sensation” in the area supplied by this root.
Brief muscle twitches are also possible. This procedure is a very safe standard procedure in anesthesia. Nevertheless, the anesthetist responsible will thoroughly explain the process and possible complications to each patient.
Areas of application
In the case of herniated discs, epidural anesthesia is used as a possible pain therapy. It should always be considered before an operation!
In contrast to pain relieving tablets, epidural anesthesia only acts locally on the affected nerve roots and does not burden the entire body circulation. During its duration of action, pain-related cramps in the muscles and vessels can be released. This often results in the pain of a herniated disc!
Under certain circumstances, a long-term application of epidural anesthesia can even be considered. To do this, the doctor connects a catheter in the epidural space with a drug pump, implanted under the skin. In this way, targeted, needs-based doses of the drug can be administered.
The epidural anesthesia is also preferred in orthopedics and gynecology. But urological interventions can also be carried out using epidural anesthesia (PDA).
Epidural anesthesia can be a useful alternative, especially for seriously ill or old patients. In contrast to a conventional general anesthetic, the entire circulation is not stressed, but only the desired nerve roots.
Typical anesthetic complications such as Respiratory arrest occurs significantly less often. Some patients are also very afraid of general anesthesia and the associated loss of control.
Frequently performed operations using a PDA are mainly:
- Use of artificial knee joints (=> knee prosthesis)
- Use of artificial hip joints (=> hip prosthesis)
- Operations on the lungs
- Operations in the abdomen, liver, pancreas, esophagus, and much more.
- Caesarean section (Cesarean section) and natural birth
Epidural anesthesia for a herniated disc
In principle, it is possible to perform epidural or epidural anesthesia even in the case of herniated discs. This is offered by special practices (e.g. specialists in neurosurgery) or hospitals, some also on an outpatient basis.
The aim is to inject pain reliever medication and, if necessary, cortisone directly into the area where the damaged intervertebral disc presses on the nerves emerging from the spinal canal. This relieves the pain and when cortisone is added, the inflammatory reaction is also inhibited.
However, this does not treat the cause, namely the compression (pressure) of the damaged intervertebral disc on the nerves. In the event of a herniated disc, patients should definitely seek advice from their family doctor and, if necessary, a specialist in orthopedics, neurosurgery or spinal surgery about the various treatment options.
Do you have a herniated disc? - Then find out about that Consequences of a herniated disc
Epidural anesthesia for a caesarean sectionIn the case of a caesarean section (Caesarean section), spinal anesthesia is usually preferred, as this offers a faster onset of action.
However, epidural or epidural anesthesia is also one of the established standard procedures that are often used in obstetrics. Epidural anesthesia is advantageous if an epidurally located catheter (PDK) has already been inserted before or during obstetric pain therapy. A sufficient dosage can then be achieved in good time so that the epidural anesthesia can be used for the planned caesarean section.
Are you about to have a caesarean section? - Then the following articles could be of interest to you:
- Spinal anesthesia during a caesarean section
- Caesarean section on request
- Pain after a caesarean section
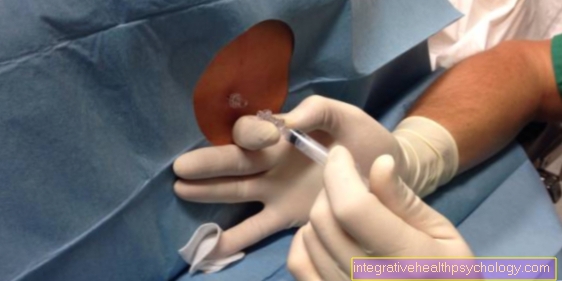
execution
The epidural anesthesia is performed under sterile conditions. This means that the doctor must do a surgical hand disinfection and all materials that come into contact with the patient's body (especially the needle) must be sterile - that is, guaranteed without the build-up of pathogens. In addition, the area around the puncture site is masked with a sterile cloth that leaves a hole free at the puncture site.
At the beginning of the epidural anesthesia, the doctor palpates two spinous processes of the spine on the back of the seated patient - at which height of the spine this happens depends on the height at which the procedure takes place later. For example, for an operation in the upper abdomen, the spinous processes of the lower thoracic spine are palpated. After the puncture site found in this way has been disinfected again, a local anesthetic agent is first injected under the skin between the two spinous processes. Then a so-called Tuohy needle is inserted into the so-called epidural space in the same place through the various layers of skin and parts of the ligamentous apparatus of the spine - hence the name epidural anesthesia.
The epidural space is a space rich in fatty tissue and blood vessels that surrounds the spinal cord and its protective covering, the meninges. In order to determine the correct penetration depth, the doctor places a syringe with liquid on the needle before inserting the needle and exerts slight pressure on the syringe during insertion. As soon as the resistance decreases noticeably, the doctor knows that he has pierced the necessary skin and ligament layers and that the tip of the needle is now in the epidural space. A local anesthetic such as Bupivacaine can be injected into the epidural space. This spreads upwards and downwards in the epidural space and develops its numbing effect after a period of approx. 20-30 minutes in the corresponding areas of the body.
The Tuohy needle can then be removed and the puncture site can be supplied with plasters, thus ending the epidural anesthesia. Alternatively, however, there is also the possibility of pushing a small plastic tube into the epidural space through the hollow interior of the needle.
This so-called catheter can remain on the patient for days and thus offers the possibility of long-term pain inhibition by means of epidural anesthesia. A pump connected to the catheter ensures that the medication is supplied evenly. Under certain circumstances, the patient can even be instructed to operate the pump himself, so that he can vary the dose of the administered medication depending on the current pain intensity, which in particular serves the purpose of early restoration of the patient's mobility and thus counteracts the development of joint stiffness and similar complications can.

The epidural anesthesia is usually carried out shortly before the operation. This happens in direct connection with further preparations for the operation by the anesthesia team, e.g. the application of the EKG and the monitoring of the oxygen level in the blood.
Opioids for epidural anesthesia
The epidural or epidural anesthesia is usually not carried out as a single-shot procedure (only a single injection). Much more often, a thin plastic catheter is positioned and fixed after the puncture, which can also be used to administer medication after the operation.
In this way, patients may have the option of receiving what is known as patient-controlled epidural anesthesia (PCEA). This is a "pain pump" in which the individual doses, the total dose and the blocking times are specified. The patient can re-dose himself as needed.
In general, opioids (strong pain relievers) are often added to the local anesthetic (local anesthetic). This saves local anesthetics. This means that the ability to move is less or not restricted at all. Thus it is then possible for the patient to walk safely. However, all patients with an attached PDK (epidural catheter) or during and after epidural anesthesia should only get up after consulting a doctor and / or nursing staff.
When should epidural anesthesia not be performed?
The list below contains contraindications for the use of epidural anesthesia (PDA). In individual cases, however, it is always necessary to clarify with the anesthetist to what extent there are concerns about performing a PDA. The PDA should not be used with:
- Blood clotting disorders
- Infections / skin diseases in the area of the injection area
- Severe cardiovascular disease
- Anemia (so-called hypovolemia)
- Increase in intracranial pressure
Read more on the topic: Xarelto®
Are there alternatives to epidural anesthesia?
The epidural anesthesia is in implementation and effect of Spinal anesthesia closely related. For all interventions below the costal arch, the epidural anesthesia can easily be replaced by a spinal anesthesia. Also with the Pain therapy Spinal anesthesia is used in the days after the operation. Here, however, the risk of cerebral fluid loss and infections is higher with continuous drug administration, which is why the PDA (epidural anesthesia) should be given preference.
Unless there are specific contraindications, all operations that can be performed under epidural anesthesia can also be performed in general anesthetic make.
What is the difference to spinal anesthesia?
Both procedures belong to the regional anesthesia procedures close to the spinal cord and can be used “only” as partial anesthesia or in combination with general anesthesia / general anesthesia.
The main difference between epidural or epidural anesthesia (PDA) and spinal anesthesia is the puncture site (the puncture site). In the case of spinal anesthesia, the puncture must be performed in the area of the lower lumbar spine between two vertebrae. This is necessary because the compact spinal cord extends into the transition between the first and second lumbar vertebrae. In order not to damage this, the injection is carried out between the third and fourth or fourth and fifth lumbar vertebrae.
In this area there is no longer a compact spinal cord, only the roots of the spinal nerves. These thread-like structures are washed around by the so-called cerebrospinal fluid (brain water / nerve water). When injecting into this region (spinal anesthesia), these nerve roots are not injured because they move in the nerve water and are not injured by the needle, as they recede during the puncture due to the changed pressure conditions.
In the case of epidural or epidural anesthesia, however, the injection needle is "only" pushed forward between the two sheets of the hard meninges in the area of the spine. This means that the anesthetic can be injected directly at the level of the area to be anesthetized. With epidural anesthesia, unlike spinal anesthesia, a small catheter is often inserted and fixed. Medication for pain relief can also be given after the operation.
birth

An important area of application for epidural anesthesia is birth dar - both natural birth and birth by Caesarean section. The puncture site is selected in the lower lumbar vertebra area, i.e. at about the level at which slim people can feel the upper edge of their pelvic bones. An epidural anesthesia is only applied when the birth process has clearly started.
In principle, it is recommended that pregnant women give birth without epidural anesthesia if possible. However, if the woman expressly wishes an epidural anesthesia, this will always be carried out. The local anesthetic is usually dosed in such a way that a noticeable, but not complete, pain reduction is achieved. This has the advantage that the Labor is not completely paralyzed, which would complicate and prolong the birth process.
The advantages of epidural anesthesia during childbirth include not only the effective pain inhibition but also the fact that the mother witnesses the birth during the caesarean section, in contrast to the general anesthetic. Epidural anesthesia is also beneficial if a caesarean section or the use of a suction cup or forceps should be necessary during the birth process, as this can be started immediately due to the anesthesia that has already taken place.
Complications
Drop in blood pressure:
A possible complication of epidural anesthesia is a drop in blood pressure, as the local anesthetic causes the vessels to widen. This can be in dizziness and express discomfort.
A drop in blood pressure occurs, among other things, because normally the sympathetic Nerve fibers are responsible for constricting blood vessels (vasoconstriction). During epidural anesthesia, these nerve fibers are blocked.
Instead, the "opponent" of the nervous system predominates, namely the Parasympathetic nervous system. As a result, the blood vessels widen (vasodilation) and the blood pressure drops.
As a side effect, overheating and reddening of the affected skin areas can be observed. In order to prevent the blood pressure dropping, a fluid supply via the vein can be arranged.
However, such a situation is usually effectively prevented by continuous blood pressure monitoring and the administration of a circulatory support agent. If the dose is too high and the contraceptive is too strong, it may be necessary for the doctor to give you a labor-inducing agents or - in the case of complete anesthesia - suction bell and forceps must be used.
A headache:
Another complication of epidural anesthesia are a headache. Headaches after epidural anesthesia arise from the smallest, unwanted injury to the hard one Spinal cord skin (Latin: dura mater). So can small amounts Brain water (Latin: Liquor cerebrospinalis) escape and the strong, so-called "Post-puncture headache" cause. Young people are particularly affected. Nowadays you can reduce the risk of this side effect by using special, thin needles (atraumatic needles) be minimized. If possible, strict bed rest in a flat supine position should be maintained after the epidural anesthesia.
Limited mobility:
In addition to the sensitive nerve fibers, the motor nerve fibers are also partially blocked. In the case of epidural anesthesia of the lumbar region, you can do so Leg or pelvic muscles be blocked for a short time.
Urinary retention:
By blocking the Parasympathetic nervous system, urinary retention (urinary retention) can be observed in some cases. Sufferers are unable to empty their bladder for a short time, despite being full. Partial, must pass a Urinary catheter be laid for relief.
Itching:
Many patients suffer from unpleasant itching at the puncture site, especially when opiates have been administered in addition to the local anesthetic.
In rare cases, epidural anesthesia can lead to life-threatening complications.
Despite the usually carried out preventive intravenous fluid supply, there is a possibility of a massive drop in blood pressure. In the worst case, a circulatory collapse with cardiac arrest can occur. Patients with narrowed coronary arteries are particularly at risk (Acute coronary syndrome) or other heart disease.
If the anesthetic is accidentally injected into the blood system, Seizures or allergic reactions are observed.
If epidural anesthesia is performed correctly, the risk of spinal cord injury is virtually eliminated! Is this Spinal cord however injured, there is always the risk of one Paraplegia.
As a rule, German clinics ensure optimal, sterile conditions for epidural anesthesia. If this is not the case, bacteria and viruses can get through the puncture site into the nervous system and possibly life-threatening Meningitis (Latin: meningitis) trigger.
Very rarely, the anesthetist can mistakenly inject the anesthetic through the hard skin of the spinal cord into the spinal space. Such a "total spinal anesthesia" is a life-threatening condition, which with Respiratory and cardiac arrest goes hand in hand. Immediate emergency action must be taken.
Concerns of parents-to-be that the drugs administered during epidural anesthesia could harm the child have so far neither been clearly confirmed nor unequivocally dispelled. To what extent parts of the active ingredients administered during epidural anesthesia get into the child's bloodstream and there negative effects such as a drop in the Heart rate can cause remains unclear. On the other hand, the tension in the cervix, which is reduced by the epidural anesthesia, in combination with the pain and contractions inhibition, can be regarded as beneficial for the child.
Bowel motility
The term intestinal motility refers to the ability of the intestine to move. The sympathetic nervous system has an inhibiting influence, so the intestinal motility is reduced. In contrast, that encourages parasympathetic nervous system the motility.
With epidural anesthesia, the sympathetic nerve fibers are primarily numbed. This eliminates the inhibiting effect on the intestine - the motility increases.
In principle, it always works increased digestion hand in hand. Thus, epidural anesthesia can be applied to e.g. Patients with chronic constipation who stimulate digestion. Nevertheless, epidural anesthesia alone is not a treatment option for chronic constipation or intestinal paralysis (Latin: ileus). Instead, the increased intestinal motility should be viewed as a side effect that may be desirable.
To make the puncture easier, the patient is asked to bend their back as far as possible in a sitting position; one often speaks of "Cat hump". Alternatively, the epidural anesthesia can also be applied in the lateral position. The subsequent use of the spray disinfectant on the back is often perceived as cold, but not uncomfortable. In order to find the correct puncture site, the doctor feels anatomical structures on the back, especially the vertebral bodies of the Spine. In order to make the insertion of the puncture needle as painless as possible, the relevant skin area is Local anesthesia stunned. The doctor then pushes the puncture needle forward as far as the so-called epidural space. This is where the drug, the so-called. Local anesthetic (Narcotics), which brings about freedom from pain. In addition, a strong pain reliever (Opioid) injected.
After removing the needle, the epidural anesthesia would in principle be free of pain for a short time operative interventions guaranteed. One speaks of the so-called. "Single shot". As a rule, however, it is advisable to insert the end of a thin plastic tube (catheter) into the epidural space. Local anesthetics and opioids can be continuously supplied via this catheter using a pump. The advantage over the Single shot is that the continuous administration ensures permanent freedom from pain even in the days after the operation.
The entire facility of the Epidural anesthesia (PDA) usually takes no more than ten minutes. As a rule, it is not perceived as particularly painful.
The onset of the pain elimination begins after a few minutes.
Note: epidural anesthesia
The sensation of pain and the sensation of temperature are always at the same time. The doctor asks the patient several times to indicate whether he or she can still perceive the stimulus of a cold spray bottle and can thus ensure that the pain sensation is switched off without having to set a pain stimulus. The first sign that the epidural anesthesia is effective is the patient's legs warming up.
As the medication progresses further, there is a loss of touch and pressure sensation and then finally the muscles fail - in the case of a PDA for an operation on the knee, this would mean that the legs are no longer actively mobile.
While with a general anesthetic the patient is ventilated by a machine and is unconscious, these two functions are not impaired with epidural anesthesia. However, the combination of PDA and general anesthesia is common practice (so-called. "Combined anesthesia") and is mostly favored by the patient himself, because he does not want to consciously experience the events during the operation. The advantage of combined anesthesia is that it is a burden on the circulatory system Anesthetics can be saved (see General anesthetic side effects). This is particularly important for patients with severe pre-existing diseases of the lungs or heart (e.g. coronary heart desease, Heart failure, Heart attack, Cardiac arrhythmia, COPD, asthma).
What happens after an epidural anesthesia is applied?
In the days after the operation, the PDA system is checked daily by the anesthesiologist. The entry point of the catheter, which is covered with a plaster, is observed for signs of infection and the pump may be refilled with medication.
Info: Adjustment of the peridural catheter
The aim of the daily check-up is to dose the pain reliever in consultation with the patient so high that there is no pain, but to dose it so low that the muscle work (i.e. active mobility) is not restricted. This is of particular importance in the case of an operation in the area of the legs in order to be able to ensure early mobilization.
This connection explains when the feeling returns to the corresponding body region: The aim is to achieve a state immediately after the operation in which the patient perceives pressure sensations when touching the body region, but not pain. Technically and pharmacologically, this state can usually be reached within an hour - it should not be concealed, however, that in practice it is often difficult to achieve this fine line between sensation of touch and freedom from pain.
The great benefit of everyone Regional anesthesia procedure (Epidural anesthesia, Spinal anesthesia) In addition to optimal pain therapy, the advantages that result from early mobilization are: Shorter length of hospital stay, lower risk of developing blood clots (thrombosis, Pulmonary embolism) and lying pressure ulcers (Pressure ulcer) and greater patient comfort.
The pumps allow the patient, according to their own needs, to continuously administer medication (so-called Basal rate) to also apply pain medication via the catheter (so-called Bolus administration). The amount of the bolus dose and the time that must lie between two bolus doses are set beforehand by the doctor on the device - this avoids accidental overdosing by the patient.
This form of pain therapy can be used even if it is not related to the operation. Here, the catheter is also placed using the method described above and can be left in place for up to several months. Areas of application are e.g. inhibiting labor pain or treating cardiac painAngina pectoris).