Phlebitis in the calf
What is phlebitis in the calf?
Inflammation of the veins, also called phlebitis, describes the inflammation of the wall of veins. This mainly affects the superficial vessels of the lower extremities, as they are exposed to greater pressure. In addition to the ankles, thighs and knees, the calves in particular are affected by such phlebitis. A distinction is also made between inflammation of intact functional veins, which is then referred to as thrombophlebits, and so-called varicophlebits, i.e. the inflammation of varicose veins. The first form is much more dangerous because there is a risk of deep vein thrombosis developing.

Symptoms of phlebitis of the calf
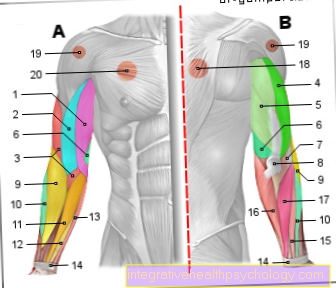
The symptoms of phlebitis are usually very characteristic. There are usually classic signs of inflammation on the calf, such as clear reddening, warming and pain. The vein can swell and harden so much that it stands out as a prominent strand from the surface of the skin. Swelling of the entire calf is rarely observed. The existing pain is clearly sensitive to pressure and becomes significantly stronger even with a slight touch. If the phlebitis is bacterial, a mild to moderate fever can occur.
Read more on the subject at: These are the symptoms you can tell if you have phlebitis
However, there are a number of other symptoms to which special attention should be paid, as they can be signs of the beginning or ongoing thrombosis of the deep veins. The most impressive symptom is probably the clear blue-red discoloration of the skin. It is an indication of the build-up of blood in the skin, since the blood can no longer flow out via the vein. The calf can swell significantly, which can be very painful. The pain will be better when the leg is raised. If there is reasonable suspicion of phlebitis, a doctor should always be presented so that adequate therapy can be initiated and a deep vein thrombosis can be ruled out.
Do you suspect that a complication has developed into a thrombosis? Then read more on the subject here: Detect thrombosis
Phlebitis pain
In the context of a phlebitis, depending on the severity of the severity, significant pain can occur. These are usually intensified by touching and applying pressure to the skin over the inflamed vein. But also when the calf muscles are tensed, especially when lifting the toes, there is a significant increase in pain. Thus, adequate pain therapy is usually part of treating phlebitis on the calf.
What are the causes?
By far the most common cause of phlebitis are varicose veins. In addition to the changed wall structure of the affected veins, there is a significantly slowed down blood flow through these vessels, which promotes the development of inflammation.
However, wearing tight clothing or long bed rest can also reduce blood flow in the leg veins and serve as risk factors. Furthermore, direct damage to the vein walls can be the cause of phlebitis. In addition to insect bites, such an injury is mostly due to medical treatment. These include, for example, taking blood, introducing a vein access or giving infusions.
Thrombosis, i.e. a blood clot in the veins, can also be the cause of phlebitis. Older people and pregnant women are particularly affected.
How is phlebitis diagnosed?
As always in medicine, the first step in any diagnosis is to collect the medical history. In particular, information about known thromboses or their risk factors, such as pregnancy or taking the pill, are decisive.
In the following physical examination, an inflamed vein usually presents itself as a red cord that shines through the skin and can be felt as severely hardened. Touching this region is usually associated with pain.
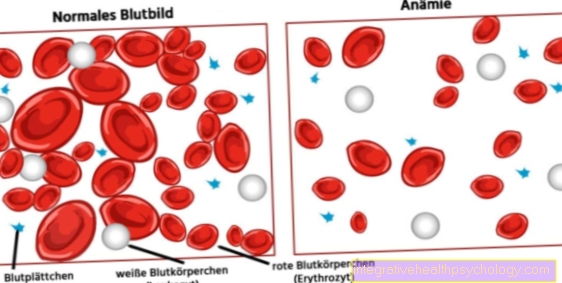
If phlebitis is suspected, an ultrasound is performed first. Here, on the one hand, the significantly thickened vessel wall with a corresponding inflammatory reaction can be detected, but also the significantly reduced blood flow. If a thrombosis can be detected on ultrasound or if it cannot be ruled out with certainty, a blood test is usually followed by further imaging, such as CT or MRI.
How is phlebitis of the calf treated?
The treatment of phlebitis in the calf initially depends on the cause and severity of the severity. If phlebitis is due to varicose veins, i.e. varicose veins, the inflammation is usually treated with cooling and anti-inflammatory and pain-relieving ointments such as diclofenac. In the second step, the varicose veins are treated.
If, on the other hand, a superficial vein thrombosis is the cause of the inflammation, in addition to cooling and the application of ointments, it is also recommended to elevate the leg and apply compression bandages. If the thrombosis, i.e. the blood clot, is fresh, in some cases it is advisable to remove it in a small outpatient procedure. However, if the thrombosis is deeper or at a branching off to a deep leg vein, there is a risk of deep vein thrombosis (DVT). In this case, blood thinning with heparin is usually attempted in order to avoid possible serious complications.
Bacterial inflammation of veins is also treated with antibiotics.
Read more on the subject at: Treatment of phlebitis
Which home remedies help with phlebitis?
There are numerous different home remedies that have been shown to be effective for superficial phlebitis over the years. Above all, this includes the use of different wraps. The most commonly used wraps are alcohol and apple cider vinegar, quark wraps or clay wraps. All of these forms promise a slight anti-inflammatory effect and cooling of the affected area, which leads to a reduction in pain.
The individual components, such as quark or clay, should have a temperature of approx. 18-23 ° C and should be applied to the wraps as thick as a finger. Depending on how tight the wrap is tied, these can also have a certain decongestant effect.
Read more on the subject at: Home remedies for phlebitis
How long does phlebitis in the calf last?
The duration of a phlebitis mainly depends on the severity of the inflammation. With adequate therapy and immobilization, milder inflammation of the vein wall usually heals after a few days, while more severe forms usually require a few weeks to be able to speak of a healing. More severe forms are usually to be expected if there is a pre-existing injury to the vein, such as after surgery or thrombosis. When the affected leg can be fully loaded again and sports activities can be carried out should always be clarified through a medical consultation.
When can you do sports again?
When and how intensively sport should be done after a phlebitis depends largely on the underlying cause.
If the inflammation is due to a varicose vein, exercising is not only tolerated but also encouraged. Since varicose veins are associated with reduced blood flow, which ultimately leads to inflammation, increased blood flow to the veins is definitely desirable during exercise. Endurance sports such as jogging or Nordic walking are particularly recommended.
In the case of thrombophlebitis, i.e. phlebitis with accompanying thrombosis, the recommendation for physical activity is dealt with more carefully. Depending on the location of the thrombus, there is a risk that it will loosen and lead to a vascular occlusion elsewhere. A sufficiently long treatment of the thrombosis should therefore be carried out and the thrombosis should be ruled out by a doctor before intensive sport should be carried out. However, light physical exercise such as walking or light Nordic walking can be carried out after consultation with the doctor.
What is the course of the disease with a phlebitis?
In the vast majority of cases, phlebitis of the calf shows a complication-free course and subsides after a few days. They usually develop within several days to weeks until they have reached their full extent and therapy is necessary. However, phlebitis can develop within hours to a few days, albeit much less frequently. This is especially the case if the vein is injured by injections, infusions or thrombosis. The further course of the disease then depends on rapid and effective therapy and usually lasts from days to a few weeks, provided the underlying cause is treated.