Glioblastoma
synonym
Glioblastoma multiforme
introduction
The Glioblastoma is the most common malignant Brain tumor in adults, due to its very poor prognosis according to the WHO classification of primary tumors of the Central nervous system as the most severe degree, so one Grade IV glioblastoma,
is classified. Glioblastoma is one of the astrocytic tumors (gliomas), which in terms of tissue (histologically) resemble the cells of the supporting tissue (glial cells) of the brain. Gliomas develop from the progenitor cells of the glial cells and are therefore brain tumors (primary brain tumors).

frequency
Glioblastoma is the most common malignant brain tumor in adults. The incidence of brain tumors in general is said to be around 50 per 100,000 inhabitants and year; among the primary brain tumors, gliomas are the most common with 4–5 new cases per 100,000 inhabitants and year. The most common glioma is glioblastoma with over 50% and accounts for about 25% of all primary brain tumors. Thus, the number of new cases of glioblastoma is approx. 3 per 100,000 inhabitants and year.
It occurs most often between the ages of 60 and 70. However, significantly younger people are also affected. Men get sick almost twice as often as women. Glioblastomas are very rare in children. Fortunately, brain tumors are rare compared to other tumors. Only around 2% of all cancer patients suffer from a brain tumor.
Occurrence
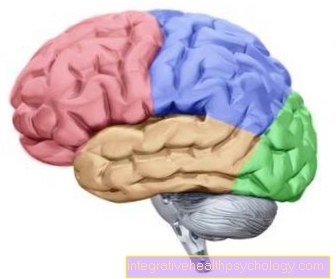
Glioblastomas grow everywhere in the central nervous system (CNS), but mostly in the Cerebrum. They start from the part of the brain that consists of nerve fibers (white matter). The tumors grow infiltrating, mostly under the cerebral cortex (subcortical), but can also grab the bark. They can be found in all cerebral lobes, but also in the so-called bar that connects the two halves of the brain (Hemispheres) connects. A glioblastoma protruding from the bar (Corpus callosum) from both sides into the anterior brain areas (Frontal lobes) will spread Butterfly glioma called. If there is extensive infiltration of the brain tissue with infestation of at least two brain lobes, one speaks of one Gliomatosis cerebri. Sometimes glioblastomas also grow along the vault (Fornix), which lies under the bar, in the Thalamus and rarely also in the middle Brain stem.
Appearance
Microscopically, the glioblastoma is characterized by multiform (multiforme) cells of different sizes and shapes with peculiar nuclei. Many of the cells are in the cell nucleus division (mitosis). The rapid growth of the tumor and the release of a vessel-forming factor that is produced by the tumor tissue lead to the formation of new abnormal (pathological) vessels with a defective wall structure. This leads to small vessel widening (aneurysms and varices), short circuits of arteries and veins (arteriovenous anastomoses) and so-called "early veins". This often leads to bleeding (apoplectic glioma) and malnutrition of the tumor, which leads to the death of active cells (necrosis) within the tumor. These necrotic tumor areas are often surrounded by pseudopallisades, which consist of linearly arranged, newly forming (neoplastic) cells.
In addition, tissue swelling develops due to the accumulation of fluid from the vascular system around the tumor (peritumoral edema), which often leads to swelling of the entire hemisphere.
causes
A glioblastoma can be primary (mostly older patients), but also secondary due to the progressive growth (progression) of one Astrocytoma WHO grade III arise (mostly middle-aged patients). Astrocytomas develop from specific glial cells called astrocytes and, like glioblastomas, belong to the group of gliomas.
The role of genetic factors in the development of Brain tumors has come more and more to the fore in recent years. The main distinguishing feature of patients with secondary glioblastoma is a change in the p53 protein (p53 mutation) that controls the cell cycle (tumor suppressor) and a loss of genes (allele loss) on chromosome 17. They are also 10 to 20 years younger than patients with primary glioblastoma, in which there is typically an EGF receptor gene duplication (amplification) or an excessive production (overexpression) of the EGF receptor. The EGF receptor serves as a docking point for the epidermal growth factor (Epidermal Growth Factor), which acts as a signaling molecule in the cell cycle. Glioblastomas are genetically very different (heterogeneous) and have a loss of a gene (deletions) in around 20% and gene duplications in a good 50%. The most common finding is a loss of genes on chromosome 10 in three quarters of all cases.
For the majority of brain tumors, however, genetic factors play no role. Environmental factors also only play a subordinate role. The vinyl chloride in the plastic PVC can be cited as an example of an influencing environmental factor.An inheritable genetic factor can be observed in the rare hereditary diseases Li-Fraumeni syndrome and Turcot syndrome. Glioblastomas occur in families here.
Risk factors for glioblastoma
The causes of glioblastoma have not been fully understood. The vast majority of glioblastomas develop spontaneously, i.e. randomly. However, a high radiation exposure could be identified as a risk factor. There are also rare genetic diseases in which those affected generally have an increased risk of tumors, e.g. the Li Fraumeni Syndrome. Diseases of this kind are also considered a risk factor for developing glioblastoma. In addition, it is not uncommon for grade 3 brain tumors to become more malignant over time and thus a glioblastoma (grade 4) can develop. This process is called malignant progression. On the basis of another brain tumor, a glioblastoma can develop even under therapy. One then speaks of one in technical terms secondary glioblastoma.
Symptoms
The first clinical symptoms appear after a few weeks or earlier. a headache (35%), epileptic seizures (30%) and psychological changes (16%) are the most common initial symptoms. A increased intracranial pressure due to the space-occupying effect of the tumor and the associated disturbance of the cerebral flow (liquor circulation) cause headaches, nausea, Vomit and swelling (edema) of the exit point of the optic nerve (congestive papilla), which can lead to impaired vision. Paralysis can also occur from the spread of the tumor. Seizure-like worsening of symptoms are due to hemorrhage from the tumor (apoplectic glioma) and are not uncommon.
You can find further information under our topic: Brain tumor signs.
diagnosis
In computed tomography (CT), glioblastomas are characterized by different densities, blurred tumor boundaries, central necrosis within the tumor and large edema around the tumor (peritumoral edema). After the administration of the contrast agent, a substance that increases the image contrast, the contrast agent accumulates, especially in the peripheral zone of the tumor. With small tumors a ring structure becomes visible, with larger ones a garland formation. Tumor hemorrhages can be seen in approx. 7% of glioblastomas.
In the MRI of the brain you can see the spread of the tumor, partly over the bar. After contrast agent administration, the contrast agent accumulates in the solid tumor parts. The typical MRI image of glioblastoma also includes residual bleeding and extensive, finger-shaped peritumoral edema. Differentiating it from a large, necrotic brain metastasis and from a brain abscess can be difficult.
Angiography can also be performed, but is no longer a standard in the diagnosis of glioblastomas. Contrast media is injected into the blood vessels and the vessels are displayed using diagnostic imaging methods such as X-rays or MRI. Angiography in glioblastomas reveals an accumulation of the contrast agent in the pathological vessels in 60–70% of cases. The veins draining from the tumor are already shown during the arterial phase ("early veins"), which shows the rapid flow of blood into the veins through the arteriovenous anastomoses.
Read more about angiography here
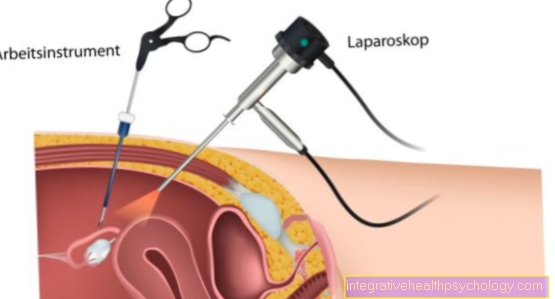
The final diagnosis of the type of tumor is made in the tissue (histologically). In the case of many inoperable tumors, histological confirmation of the type of tumor is desirable before irradiation. The brain biopsy, in which a very small piece of brain tissue is cut out, is either carried out openly at the same time as tumor reduction or under local anesthesia minimally invasive, i.e. with the smallest injury.
You might also be interested in: Brain biopsy and End-stage glioblastoma
MRI of the brain - what do you see?
A glioblastoma is often suspected using an imaging test. Most often this is magnetic resonance imaging. The typical finding shows a tumor without a homogeneous (uniform) structure. The solid parts (solid parts) are very well supplied with blood and therefore absorb a lot of contrast medium. This is obvious at first glance. They are very bright and literally glow on the MRI image. There are also recesses for contrast medium (areas that do not appear bright in the MRI). These are cystic parts or dead cell aggregates (necroses), these are not supplied by a blood vessel and therefore cannot absorb contrast media. The tumor is usually immediately seen as an edema (swollen cells). The space-consuming effect of the tumor can often be recognized at the initial diagnosis, i.e. the midline is already displaced by the tumor growth. However, for the final diagnosis, a sample must be taken and examined under a microscope. Only the pathologist can confirm the diagnosis of glioblastoma with certainty.
Read more at: MRI of the brain
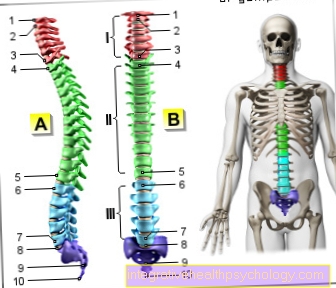
WHO - grade
The World Health Organization (WHO) divides brain tumors into 4 groups based on their growth behavior. Grade 1 tumors grow slowly and are considered benign. Grade 4 tumors grow extremely quickly and have a very poor prognosis. Grade 2 and 3 tumors are in between. A Glioblastoma is a tumor that originates from the supporting or envelope cells of the nerve cells, these are called in technical jargon Glial cells called. Hence the name. Due to its rapid growth and poor prognosis, glioblastomas are grade 4 tumors.
Grade 1 and 2
While grade 1 tumors are referred to as benign brain tumors by the WHO, malignant cells can be detected in grade 2 tumors. In 50% of grade 2 tumors, a new tumor with a higher level of malignancy (grade 3-4) develops, so life expectancy is also limited. Similar to the gliobastoma, these tumors also originate from the supporting or envelope cells of the brain. In contrast to glioblastoma, a grade 4 tumor, grade 2 brain tumors grow much more slowly and have a significantly better prognosis.
Grade 3
According to the World Health Organization (WHO) classification, grade 3 tumors are malignant, rapidly growing brain tumors. The prognosis is bad. Despite therapy, many patients die after 2-3 years. Typical grade 3 tumors are so-called anaplastic astrocytomas; like the glioblastomas against them from the supporting and envelope cells of the nerve cells. Glioblastomas are, however, a group 4 tumor due to their even faster growth. Despite maximum therapy, the mean survival time is approx. 1 year.
Grade 4
Grade 4 tumors are even more malignant, grow faster and lead to a significant reduction in life expectancy despite therapy. The classification of the tumor into the corresponding WHO grade therefore strongly influences the prognosis of the patient. Glioblastomas are always grade 4 tumors with a very poor prognosis. Of course, other factors such as operability, location and response to chemotherapy and / or radiation therapy also play an important role when it comes to the patient's prognosis. The mean survival time for glioblastoma averages one year after diagnosis.
Read more at: Grade 4 glioblastioma
Life expectancy / prognosis
Unfortunately, glioblastoma is very difficult to treat. A permanent cure is usually not possible. Ultimately, the patient usually dies from the tumor. The standard therapy consists of surgery followed by radiation and chemotherapy. Unfortunately, the tumor grows very quickly and infiltrates the surrounding nerve tissue, so that all tumor cells can never be removed during an operation. The tumor usually comes back (Relapse). With the following figures on prognosis and life expectancy, one should be aware that these are statistics, in individual cases the actual survival time of the patient can vary widely.
Young patients (age <50 years) with good surgical results have the best prognosis. 70% survive the first year. The median survival time after diagnosis is 17-20 months. Only about 15 percent are still alive after 5 years. The prognosis worsens with age. In patients over 50 years of age or in younger patients with significant limitations, the mean survival time is often just under a year despite the good surgical result. In patients without surgery or with poor neurological function postoperatively, the prognosis is even worse. Only a third survive the first year. The average dies after 8 months. Individual patients have a relatively good quality of life despite relapse and survive for several years regardless. So far, however, these have been isolated cases. Which factors favorably influence the prognosis is therefore intensively researched.
Read more on the topic: Glioblastoma - course of the individual stages
What is the course of a glioblastoma?
Glioblastoma is a malignant tumor in the brain with a very poor prognosis. A cure is usually not possible. Patients die on average about 1 year after diagnosis. If the position of the tumor is favorable and the general condition of the patient is good, surgical removal is carried out first. Unfortunately the glioblastoma grows so infiltrating into the nervous tissue that all tumor cells can never be removed. The operation is therefore followed by radiation and chemotherapy. However, this can only delay the natural course of the disease. Except in rare individual cases, the tumor returns (Relapse). It usually grows so quickly that the increased pressure on the brain soon causes symptoms such as nausea / vomiting and severe headaches. Disturbances in consciousness follow. The increasing intracranial pressure then ultimately traps certain areas of the brain. If the brain stem is affected, respiratory paralysis and death are the result. The above treatment can delay this for a few months, but the course of the disease is unstoppable and ends in death.
Read more on the subject at: Course of a glioblastoma
What does the end stage look like?
Glioblastoma is a malignant tumor from which patients usually die. A cure is currently not possible - despite surgery, radiation and chemotherapy. In the end, it is difficult to pinpoint when the terminal stage is reached. Usually the tumor grows again after the operation (Relapse). This is often no longer operable. Sometimes the tumor is so large or unfavorably localized at the time of diagnosis that it cannot be operated on at all. As a grade 4 tumor, glioblastoma is characterized by rapid growth. In the final stage, the tumor is very large. However, there is only limited space in the bony skull. The pressure on the brain increases. With increased intracranial pressure, patients then suffer from nausea and vomiting as well as severe headaches. Disturbances of consciousness up to a coma are possible. Patients are often sleepy and confused. Due to the increasing intracranial pressure, there is also the risk that certain brain regions will be pinched by too much pressure in the skull.
Read more on the topic: Increased intracranial pressure - signs, causes, and treatment
As with most end-stage cancers, patients are often emaciated from the long duration of the disease. You feel limp and exhausted, you may not even be able to get out of bed. One then tries to alleviate the suffering somewhat by prescribing strong painkillers to the patient. The patient also receives medication against nausea. A palliative care should be done.
You might also be interested in: End-stage glioblastoma
Metastases
Metastases spread the cancer throughout the body. One also often hears the words the tumor has spread. One speaks of it when the tumor has formed daughter lumps in another part of the body. Glioblastoma is a rapidly growing malignant brain tumor. It grows infiltratively, i.e. it spreads in both the brain and the meninges. About the nerve water (Liquor) the tumor cells are distributed throughout the central nervous system (brain and spinal cord) and can settle again anywhere. Daughter tumors rarely develop outside of the central nervous system.
Changes in nature due to the tumor
Every cancer represents a significant turning point in the life of the person affected. The processing of the diagnosis glioblastoma varies greatly from person to person, but this diagnosis alone is a massive psychological burden. The sudden confrontation with the fact that one's life is finite changes most people. In addition, the personality is stored in the brain, especially in the front part of the brain, the so-called Frontal lobes. Tumors that grow there can lead to organic changes in nature, as they displace your own brain tissue. Unfortunately, patients are usually aggressive and abusive for no reason. That is an extreme burden for the environment. Due to the increasing intracranial pressure in the end stage of the disease, the patients are usually listless and tired.
Can you cure a glioblastoma?
Unfortunately, this question has to be answered with a clear no. The median survival time after diagnosis is one year. Of course, the individual case can differ considerably from the statistics. Young patients (under 50 years of age) in particular have a slightly better prognosis. They survive on average about 18 months. There are also isolated cases of patients who are still alive after 5 years. It is possible that there are a few patients around the world who are still alive 10 years after the diagnosis, but it is certainly the absolute exception. At the current state of science, a cure for glioblastoma is not possible. Numerous research approaches are being pursued, but so far it is unlikely that such a breakthrough therapy will be discovered in the next few years that could lead to a cure for the tumor. In all studies so far only an increase in survival time in months could be achieved.
What is a multiform glioblastoma?
The term multiform literally means "diverse", I.e. related to the tumor, that the tumor is characterized by a diverse appearance. This term comes from pathology. However, even the inexperienced doctor can already see in the MRI image that the tumor does not have a uniform structure. Under the microscope you can see hemorrhages and necroses (= dead cells). Every glioblastoma is by definition a multiformed tumor. This inhomogeneous (uneven) composition characterizes the glioblastoma.
therapy
The therapy consists of the most radical surgical removal of the tumor and the subsequent irradiation with a total dose of 60 Gray (30 individual fractions - 2 Gy / 5 days / week for 6 weeks). The edema responds well to steroid treatment, for example Dexamethasone, on. With radiation and anti-edematous therapy, a clinically impressive improvement can initially occur. A renewed occurrence or growth (relapse) of the tumor is inevitable. The main prognostic factors are: age and extent of clinical impairment at the start of therapy.
Also chemotherapy becomes increasingly with the radiation, especially with the substance Temozolomide, combined or used subsequently. Nevertheless, the chances of therapy in glioma patients are low, the one-year survival rate for glioblastoma multiforme is 30–40%. The chemotherapy with Nitrous ureas (BCNU, CCNU) leads to a slight life extension of only a few weeks to months. An alternative to the nitrous ureas is temozolomide, which has fewer side effects and can be administered on an outpatient basis as an oral cytostatic, an agent that inhibits cell division. The combined radiation and chemotherapy with temozolomide leads to an extension of the lifetime to 14 months (without temozolomide: 12 months) and an increased two-year survival rate of 26% (without: 10%). Young patients under 45 years of age in good health seem to benefit most from this therapy.
Temozolomide is also used in the treatment of recurrence of malignant gliomas. Relapse therapy leads to a stabilization of tumor growth in about 50% of the patients and to an overall survival time of 13 months after the start of relapse therapy.
Who can be operated on?
Surgical removal of a glioblastoma is decided when the tumor is easily accessible and removable due to its location. Usually there are already indications of the rapid growth of the tumor; one can see in the sectional imaging that the surrounding tissue is displaced. This is called a space-consuming effect. Last but not least, the general condition or ability of the patient to be anesthetized is decisive for the decision to have an operation. Tumors that are too close to important brain regions cannot be operated on. For example, if the speech or respiratory center is right next to the tumor, an operation is not possible or useful. Then the tumor is considered to be inoperable.
Irradiation
Surgery can never remove all of the tumor cells; isolated tumor cells are still present. These can grow back into a large tumor. In order to prevent this or at least kill as many remaining tumor cells as possible, radiation treatment follows after the operation. Not only is the original tumor area irradiated, but also a safety margin of 2-3 cm. Sometimes the patient receives chemotherapy in parallel with radiation.
Read more on the topic: Treatment with radiation therapy
chemotherapy
In addition to surgery and radiation, chemotherapy is standard therapy for glioblastomas. As the tumor infiltrates the brain tissue every week, all tumor cells can never be removed during the operation. Therefore, chemotherapy can extend relapse-free survival by at least a few months. Temozolomide is the chemotherapy drug of choice. It is good at crossing the blood-brain barrier. It is available in tablet form and can be taken at home. In addition, it has relatively few side effects and is well tolerated.
Immunotherapy
In the fight against malignant tumors these days are increasing Immunotherapeutics used. But what does the term immunotherapy actually mean?
Immunotherapy involves influencing the body's own immune system with drugs to kill tumor cells. It is actually a collective term for numerous different approaches. Glioblastoma is a very rapidly growing malignant brain tumor that, despite maximum therapy, is associated with a very poor prognosis. Hence, much hope rests on immunotherapy. There are also very promising approaches in this area, which are currently being intensively researched in clinical studies.
Methadone
Many patients and relatives now have new hope through media reports about methadone. But what are the facts? In the laboratory it has been shown that methadone reacts better to chemotherapy and is thus killed more effectively.
However, a study carried out at the Charité in Berlin on 27 patients could not show any survival benefit for the group treated with methadone. However, other colleagues repeatedly report individual cases in which patients with methadone live 2-3 years longer without recurrences. It is therefore currently very difficult to make a recommendation. First laboratory results and individual case reports speak in favor of methadone. So far, however, there are no high-quality clinical studies with large patient populations. You can certainly only count on these data in about 3 years. Before that, it is not possible to make a scientifically sound statement about the importance of methadone in cancer therapy. Affected patients have the opportunity to discuss with their treating doctor whether methadone is considered off label therapy nevertheless cannot be prescribed in the sense of an experimental healing attempt. An off-label therapy means that the doctor prescribes a drug for the patient, although it is not approved for the treatment of a certain disease. Methadone is an old drug that has been tried and tested for a long time. So far, however, it has not been approved to supplement chemotherapy for glioblastoma because there are no valid data to prove its effectiveness.
For more information on the use of methadone to treat addiction, read the following article: Therapy of an addiction
When do you need cortisone?
Water retention (Edema) around the tumor are often part of the disease, especially in the end stage of glioblastoma. This leads to a swelling of the nerve cells and thus increases the intracranial pressure. So-called brain edema is a potentially life-threatening disease. Cortisone is needed to counteract cerebral edema. It stabilizes the cell walls, the cells no longer absorb fluid in an uncontrolled manner and lose size again. The brain swells. This happens within a few hours after administration of cortisone. Therefore, cortisone is often a vital drug for the patient.
epilepsy
Half of all patients with glioblastoma also develop epileptic seizures. The seizures can sometimes even be the first sign of the tumor leading to the diagnosis. If the tumor is then surgically removed, the risk of seizures initially drops significantly. Basically, however, patients with a brain tumor have a significantly increased risk of epilepsy, so after the first attack, drug prophylaxis should definitely be started in order to reduce the risk of further attacks.
Read more on the topic: Brain tumor signs
Is Glioblastoma Hereditary?
Fortunately, in most cases this question can be answered with a resounding no. Even if a relative, e.g. If one of your parents developed a glioblastoma, you are not at a higher risk of developing this brain tumor than the general population. Glioblastoma is a sporadic tumor, i.e. the tumor occurs randomly, there is no evidence of heredity. However, there are rare genetic diseases in which there is generally an increased risk of malignant tumors, e.g. the Li Fraumeni Syndrome or that Turcot Syndrome. Glioblastomas can of course also occur more frequently in affected families.
























-und-lincosamine.jpg)